Achalasia - series
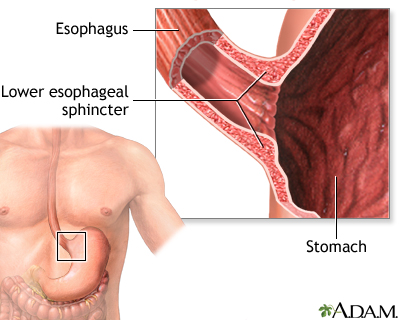
Normal anatomy
The esophagus carries food from the mouth to the stomach. The lower esophageal sphincter is a muscular ring at the junction of the esophagus and the stomach. The lower esophageal sphincter relaxes when food from the esophagus enters the stomach.
Indications
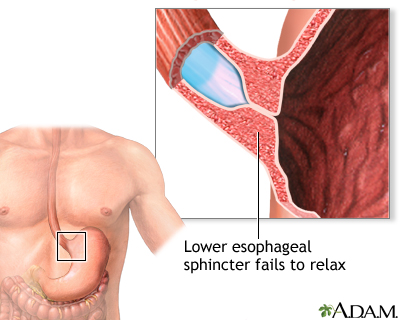
Achalasia is a disorder in which the esophageal sphincter does not relax when food passes down the esophagus to the stomach. As a result, the esophagus becomes distended and filled with food, and food passes into the stomach very slowly.
Achalasia is often associated with chest pain during eating, weight loss, and regurgitation of food. The esophagus becomes distended as food and liquid are unable to pass into the stomach.
Procedure, part 1
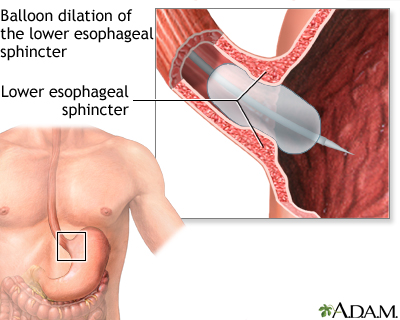
Achalasia can sometimes be treated with medication that helps the lower esophageal sphincter relax. If medication is ineffective, however, esophageal dilatation can correct the problem.
To open the esophagus, a balloon dilator is passed through the mouth down to the level of the lower esophageal sphincter, using an endoscope. The balloon is inflated, thus stretching the sphincter.
Incision
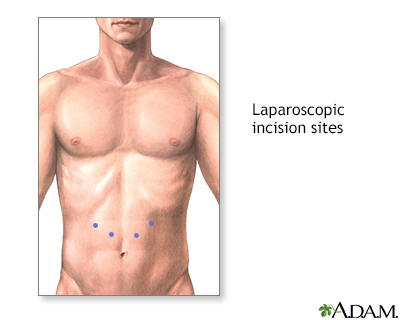
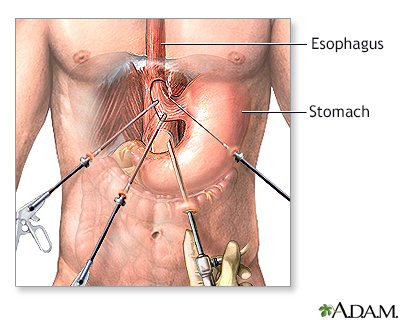
If achalasia recurs after balloon dilatation, surgery may be necessary to correct the defect. This surgery can often be done laparoscopically.
Laparoscopic surgery involves a number of small incisions made in the upper abdomen, into which the surgeon inserts a long, thin camera and surgical instruments.
Procedure, part 2
The surgeon then makes a long incision in the esophagus at the level of the esophageal sphincter. This releases the sphincter and allows it to relax. This surgery is very effective in curing achalasia, with over 90% of patients obtaining relief from symptoms post-operatively.
Recovery is generally rapid, and most patients are able to leave the hospital within 1 to 3 days. Infrequently, the operation cannot be accomplished laparoscopically, and a larger incision is required. In these cases, hospitalization times may be longer.
BACK TO TOP
Review Date: 12/31/2023
Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
