Anterior vaginal wall repair (surgical treatment of urinary incontinence) - series
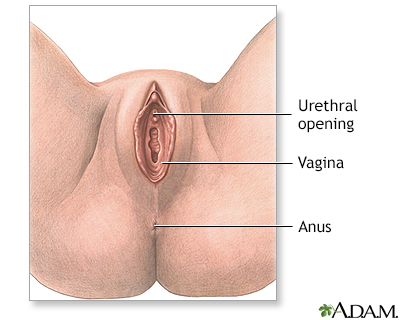
Normal anatomy
The vaginal opening lies just below the urethral opening, and just above the anal opening. The urethral opening, through which urine passes, leads to the bladder. The anus leads to the rectum. The vaginal opening leads to the vaginal canal, which leads to the uterus.
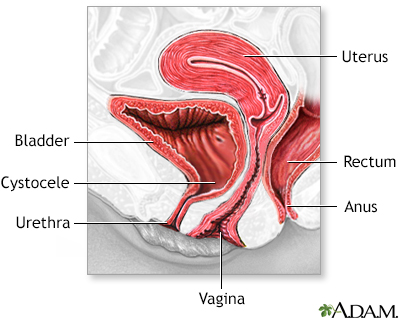
Indications
This procedure is used to repair the vaginal wall herniation that occurs with urethrocele, cystocele, or rectocele. This is occasionally performed to treat stress incontinence in women by supporting the bladder and urethra in its proper position, so it can function properly. As with most other surgical procedures, it is advised that you try medicines and bladder retraining therapy first, before resorting to surgical treatment.
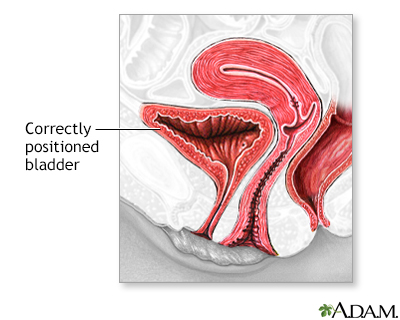
Procedure, Part 1
To perform the anterior vaginal repair, an incision is made through the vagina to release a portion of the anterior (front) vaginal wall that is attached to the base of the bladder. The bladder and urethra are then stitched into the proper position. There are several variations on this procedure that may be necessary based on the severity of the dysfunction. This procedure may be performed using general or spinal anesthesia. You may have a foley catheter in place for one to two days after surgery. You will be given a liquid diet immediately after surgery, followed by a low residue diet when your normal bowel function has returned. Stool softeners and laxatives may be prescribed to prevent straining with bowel movements since this can cause stress on the incision.
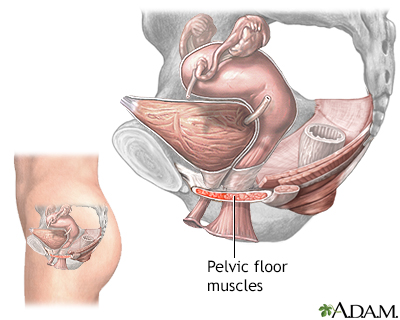
Procedure, Part 2
Women treated with this procedure have approximately a 60% rate of success in relieving symptoms. You should avoid activities that cause an increase in abdominal pressure, such as straining, sneezing, and coughing. Try to tighten your pelvic muscles when coughing or sneezing to support the bladder. You may need to urinate at least every 2 to 3 hours, or perform clean intermittent self catheterization (CISC), to keep your bladder from getting too full and putting pressure on the stitches. You should avoid any activities that require lifting or straining. You may need to take stool softeners or gentle laxatives to prevent constipation and straining with bowel movements.
BACK TO TOP
Review Date: 5/17/2024
Reviewed By: Sovrin M. Shah, MD, Associate Professor, Department of Urology, The Icahn School of Medicine at Mount Sinai, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
