Gallbladder removal - Series
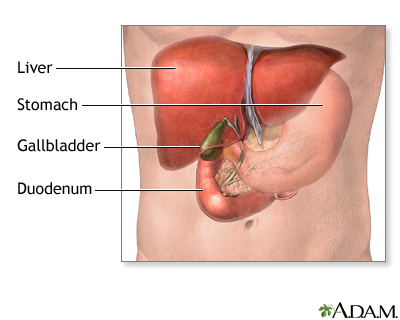
Normal anatomy
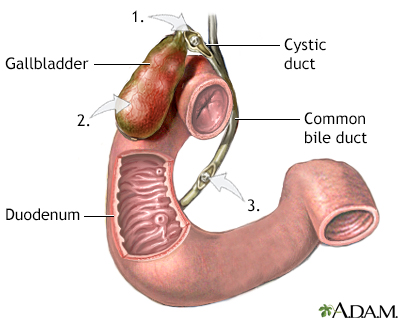
The gallbladder is located in the abdomen, on the right side, underneath the liver. The gallbladder stores bile produced by the liver, and delivers it to the first part of the small intestine (duodenum), where it aids in the digestion of fat. The cystic and common bile ducts connect the gallbladder to the duodenum-bile passes through these ducts from the gallbladder to the duodenum.
Indications
Gallbladder surgery is done to treat gallbladder disease. Gallbladder disease is commonly caused by the formation of gallstones in the gallbladder (cholelithiasis). Gallstones can affect different locations.
- Obstruction of the cystic duct leading to severe abdominal pain (biliary colic).
- Infection or inflammation of the gallbladder (cholecystitis).
- Blockage of the biliary ducts leading to the duodenum (biliary obstruction).
In each case, the gallbladder is often removed (cholecystectomy).
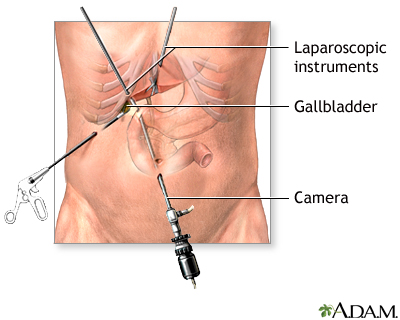
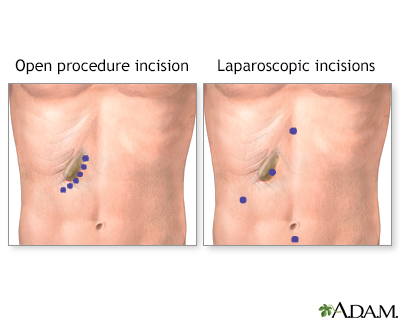
Incision
Most gallbladder surgery today is done using laparoscopic surgical techniques, in which narrow instruments, including a camera, are introduced into the abdomen through small puncture holes. If the procedure is expected to be straightforward, laparoscopic cholecystectomy may be used. A laparoscopic camera is inserted into the abdomen near the umbilicus (navel). Instruments are inserted through 2 more small puncture holes. The gallbladder is found, the vessels and tubes are cut, and the gallbladder is removed.
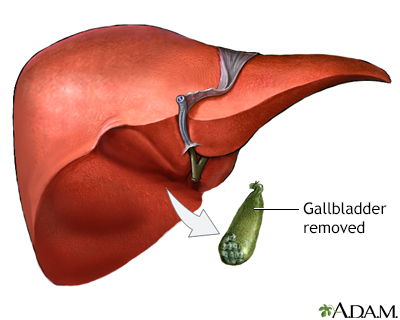
Procedure
If the gallbladder is extremely inflamed, infected, or has large gallstones, the abdominal approach (open cholecystectomy) is recommended. A small incision is made just below the rib cage on the right side of the abdomen. The liver is moved to expose the gallbladder. The vessels and tubes (cystic duct and artery) to and from the gallbladder are cut and the gallbladder is removed. The tube (common bile duct) that drains the digestive fluid (bile) from the liver to the small intestine (duodenum) is examined for blockages or stones. A small flat tube may be left in for several days to drain out fluids if there is inflammation or infection.
Aftercare
Most patients who undergo laparoscopic cholecystectomy can go home the day of surgery or the next day, and resume a normal diet and activities immediately. Most patients who undergo open cholecystectomy require 5 to 7 days of hospitalization, are able to resume a normal diet after one week, and normal activities after 4 to 6 weeks.
Related Information
GallstonesAcute cholecystitis
Open gallbladder removal
BACK TO TOP
Review Date: 9/9/2023
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
