Exchange transfusion - series

Procedure
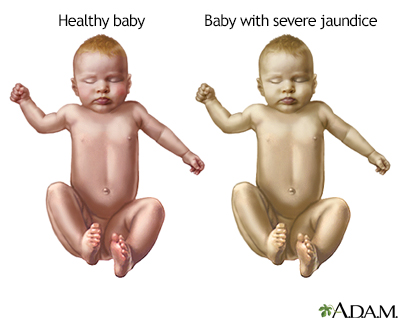
Neonatal jaundice is a common problem among infants immediately after birth. It is the result of the inability of the neonatal liver to clear bilirubin, a breakdown product of blood cells, from the blood. Neonatal jaundice is usually a self-limiting, mild disorder. The most commonly used treatment is fluorescent light exposure, in which the infant is placed under a lamp for a few hours each day. The blue light breaks down bilirubin into a form the infant liver can process and eliminate.
Indication
Less frequently, when neonatal jaundice is more severe, and fluorescent light therapy is unable to break down all circulating bilirubin, exchange transfusion is often used. High levels of bilirubin in the blood can lead to brain damage and other serious problems. In these cases, exchange transfusion is a life-saving procedure designed to counteract the effects of serious jaundice, infection, or toxicity. The procedure involves the staged removal of the infant's blood and replacement with fresh donor blood or plasma.
Guidelines for an exchange transfusion include:
- Hemolytic disease of the newborn (Rh disease)
- Life-threatening infection
- Severe disturbances in body chemistry
- Toxic effects of drugs
- Polycythemia
Procedure
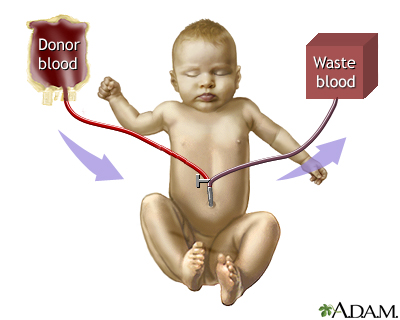
The infant is laid on his or her back, usually under a radiant warmer. The umbilical vein is catheterized with a fluid-filled catheter. The catheter is connected to an exchange transfusion set, incorporating lines to and from a waste container and a pack of donor blood. These are connected by means of a four-way stopcock, to which is also attached the syringe used to remove and replenish the infant's blood.
The exchange transfusion now goes ahead in cycles, each of a few minutes duration. Slowly the infant's blood is withdrawn, and the fresh, pre-warmed blood or plasma is injected. After the exchange transfusion, an umbilical catheter may be left in place in case the procedure needs to be repeated within a few hours.
Related Information
Exchange transfusionRh incompatibility
Newborn jaundice
Jaundice and breastfeeding
Jaundice
Bili lights
BACK TO TOP
Review Date: 1/17/2025
Reviewed By: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
