Haptoglobin blood test
The haptoglobin blood test measures the level of haptoglobin in your blood.
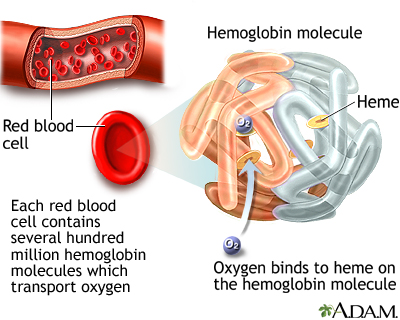
Haptoglobin is a protein produced by the liver. It attaches to hemoglobin in the blood. Hemoglobin is a blood cell protein that carries oxygen.
Images
I Would Like to Learn About:
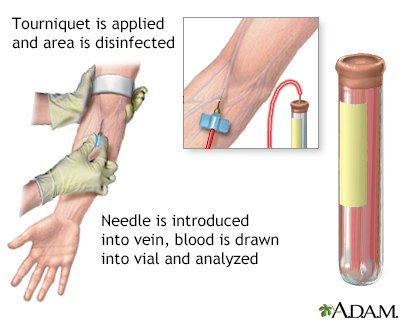
How the Test is Performed
A blood sample is needed.
How to Prepare for the Test
Certain medicines may affect the results of this test. Your health care provider will tell you if you need to stop taking any medicines. Do not stop any medicine before talking to your provider.
Medicines that can raise haptoglobin levels include:
- Androgens
- Corticosteroids
Medicines that can lower haptoglobin levels include:
- Birth control pills
- Chlorpromazine
- Diphenhydramine
- Indomethacin
- Isoniazid
- Nitrofurantoin
- Quinidine
- Streptomycin
How the Test will Feel
When the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging. Afterward, there may be some throbbing or a slight bruise. This soon goes away.
Why the Test is Performed
This test is done to see how fast your red blood cells are destroyed. It may be done if your provider suspects you have a type of anemia that your immune system is causing.
Normal Results
The normal range is 41 to 165 milligrams per deciliter (mg/dL) or 410 to 1,650 milligrams per liter (mg/L).
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Talk to your provider about the meaning of your specific test results.
What Abnormal Results Mean
When red blood cells are actively being destroyed, haptoglobin disappears faster than it is created. As a result, the levels of haptoglobin in the blood drop.
Lower than normal levels may be due to:
- Immune hemolytic anemia
- Long-term (chronic) liver disease
- Blood buildup under the skin (hematoma)
- Liver disease
- Transfusion reaction
Higher-than-normal levels may be due to:
- Blockage of the bile ducts
- Joint or muscle inflammation, swelling, and pain that comes on suddenly
- Peptic ulcer
- Ulcerative colitis
- Other inflammatory conditions
Risks
There is little risk involved with having your blood taken. Veins and arteries vary in size from one person to another and from one side of the body to the other. Taking blood from some people may be more difficult than from others.
Other risks associated with having blood drawn are slight but may include:
- Excessive bleeding
- Fainting or feeling lightheaded
- Multiple punctures to locate veins
- Hematoma (blood accumulating under the skin)
- Infection (a slight risk any time the skin is broken)
Related Information
HemoglobinAmino acids
Gout
Bile duct obstruction
Peptic ulcer
Ulcerative colitis
Liver disease
Hemolytic disease of the newborn
Hemolytic anemia
Glucose-6-phosphate dehydrogenase deficiency
Immune hemolytic anemia
Primary biliary cholangitis
Hemolytic transfusion reaction
References
Marcogliese AN, Hensch L. Resources for the hematologist: interpretive comments and selected reference values for neonatal, pediatric, and adult populations. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 159.
Michel M. Autoimmune and intravascular hemolytic anemias. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 146.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
