ACE blood test
Serum angiotensin-converting enzyme; SACE
The ACE test measures the level of angiotensin-converting enzyme (ACE) in the blood.
Images
I Would Like to Learn About:
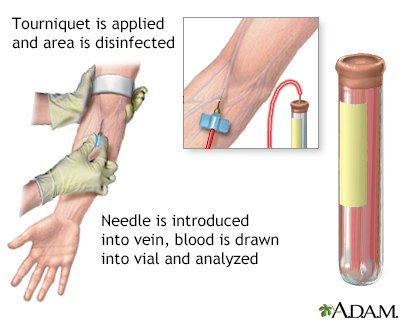
How the Test is Performed
How to Prepare for the Test
Follow your health care provider's instructions for not eating or drinking for up to 12 hours before the test. If you are on steroid medicine, ask your provider if you need to stop the medicine before the test, because steroids can decrease ACE levels. Do not stop any medicine before talking to your provider.
How the Test will Feel
When the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging. Afterward, there may be some throbbing or slight bruising. This soon goes away.
Why the Test is Performed
This test is most often ordered to help diagnose and monitor a disorder called sarcoidosis. People with sarcoidosis may have their ACE level tested regularly to check how severe the disease is and how well treatment is working.
This test may also help confirm a diagnosis of Gaucher disease.
Normal Results
Normal values vary based on your age and the test method used. Adults have an ACE level less than 40 micrograms per liter.
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Talk to your provider about the meaning of your specific test results.
What Abnormal Results Mean
Higher than normal ACE level may be a sign of sarcoidosis. ACE levels may rise or fall as sarcoidosis worsens or improves.
A higher than normal ACE level may also be seen in several other diseases and disorders, including:
- Adrenal glands do not make enough hormones (Addison disease)
- Cancer of the lymph tissue (Hodgkin disease)
- Diabetes
- Liver swelling and inflammation (hepatitis) due to alcohol use
- Lung disease such as asthma, cancer, chronic obstructive pulmonary disease, or tuberculosis
- Kidney disorder called nephrotic syndrome
- Multiple sclerosis
- Overactive thyroid (hyperthyroidism)
- Overactive parathyroid glands (hyperparathyroidism)
- Stomach ulcer
Lower than normal ACE level may indicate:
- Chronic liver disease
- Chronic kidney failure
- Eating disorder called anorexia nervosa
- Steroid therapy (usually prednisone)
- Therapy for sarcoidosis
- Underactive thyroid (hypothyroidism)
Risks
There is little risk involved with having your blood taken. Veins and arteries vary in size from one person to another and from one side of the body to the other. Taking blood from some people may be more difficult than from others.
Other risks associated with having blood drawn are slight, but may include:
- Excessive bleeding
- Fainting or feeling lightheaded
- Hematoma (blood buildup under the skin)
- Infection (a slight risk any time the skin is broken)
- Multiple punctures to locate veins
Related Information
EnzymeSarcoidosis
Leprosy
Histoplasmosis
Cirrhosis
Primary amyloidosis
Asbestosis
Diabetes
Hodgkin lymphoma
Hyperthyroidism
Idiopathic pulmonary fibrosis
Primary biliary cholangitis
Pulmonary embolus
Scleroderma
Silicosis
Pulmonary tuberculosis
References
Pincus MR, Carty RP. Clinical enzymology. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 21.
Vaidya A, Zennaro MC, Stowasser M. Primary aldosteronism. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 95.
Young WF. Endocrine hypertension. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 16.
BACK TO TOPReview Date: 11/19/2023
Reviewed By: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
