Prostate-specific antigen (PSA) blood test
Prostate-specific antigen; Prostate cancer screening test; PSA
Prostate-specific antigen (PSA) is a protein produced by prostate cells.
The PSA test is done to help screen for and monitor prostate cancer in men.
Images
I Would Like to Learn About:
How the Test is Performed
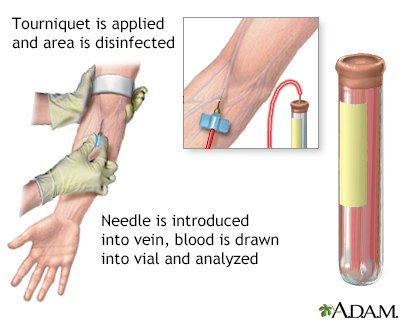
A blood sample is needed.
How to Prepare for the Test
Make sure your health care provider knows all the medicines you are taking. Some drugs cause your PSA level to be falsely low.
In most cases, no other special steps are needed to prepare for this test. You should not have a PSA test soon after having a urinary tract infection or undergoing a procedure or surgery involving the urinary system. Ask your provider how long you should wait.
How the Test will Feel
You may feel slight pain or a prick when the needle is inserted. Afterward, there may be some throbbing or a slight bruise. These soon go away.
Why the Test is Performed
Reasons for a PSA test:
- To screen for prostate cancer.
- To monitor people after prostate cancer treatment to see if the cancer has come back.
- If a provider feels the prostate gland is not normal during physical exam.
MORE ABOUT SCREENING FOR PROSTATE CANCER
Measuring the PSA level can increase the chance of finding prostate cancer when it is very early. But there is debate over the value of the PSA test for detecting prostate cancer. No single answer fits all men.
For some men 55 through 69 years old, screening may help reduce the chance of death from prostate cancer. However, for many men, screening and treatment could potentially be more harmful than beneficial. The US Preventive Services Task Force recommends against PSA-based screening for prostate cancer in men 70 years and older.
Before having the test, talk to your provider about the pros and cons of having a PSA test. Ask about:
- Whether screening decreases your chance of dying from prostate cancer
- Whether there is any harm from prostate cancer screening, such as side-effects from testing or overtreatment of cancer when discovered
Some men younger than age 55 have a higher than usual chance of developing prostate cancer and should talk with their provider about PSA screening if they:
- Have a family history of prostate cancer (especially a brother or father)
- Are African American
Normal Results
The PSA test result cannot diagnose prostate cancer. Only a prostate biopsy can diagnose this cancer.
Your provider will look at your PSA result and consider your age, ethnicity, medicines you are taking, and other things to decide whether your PSA is normal or whether you need more tests.
A normal PSA level is considered to be up to 4.0 nanograms per milliliter (ng/mL) of blood, but this varies by age:
- For men in their 50s or younger, a PSA level should be below 2.5 ng/mL in most cases.
- Older men often have slightly higher PSA levels than younger men.
What Abnormal Results Mean
A high PSA level has been linked to an increased chance of having prostate cancer.
PSA testing is an important tool for detecting prostate cancer, but it is not foolproof. Other conditions can cause a rise in PSA, including:
- A large prostate
- Prostate infection (prostatitis)
- Urinary tract infection
- Recent tests on your bladder (cystoscopy) or prostate (biopsy)
- Catheter tube recently placed into your bladder to drain urine
- Recent intercourse or ejaculation
- Recent colonoscopy
Your provider will consider the following things when deciding on the next step:
- Your age
- If you had a PSA test in the past and how much and how fast your PSA level has changed
- If a prostate lump was found during your exam
- Other symptoms you may have
- Other risk factors for prostate cancer, such as ethnicity and family history
Men at high risk may need to have more tests. These may include:
- Repeating your PSA test, most often sometime within 3 months. You may receive treatment for a prostate infection first.
- A prostate biopsy if the PSA level is persistently high, or if the level keeps rising when the PSA is measured again.
- A follow-up test called a free PSA (fPSA). This measures the percentage of PSA in your blood that is not bound to other proteins. The lower the level of this test, the more likely it is that prostate cancer is present.
Other tests may also be done. The exact role of these tests in deciding on treatment is unclear.
- A urine test called PCA-3.
- An MRI of the prostate may help identify cancer in an area of the prostate that is hard to reach during a biopsy.
If you have been treated for prostate cancer, the PSA level can show if treatment is working or if the cancer has come back. Often, PSA level rises before there are any symptoms. This may happen months or years beforehand.
Risks
There is little risk involved with having your blood taken. Veins and arteries vary in size from one person to another, and from one side of the body to the other. Taking blood from some people may be more difficult than from others. Other risks associated with having blood drawn are slight, but may include:
- Excessive bleeding
- Multiple punctures to locate veins
- Fainting or feeling lightheaded
- Hematoma (blood accumulating under the skin)
- Infection (a slight risk any time the skin is broken)
Related Information
Prostate cancerEnlarged prostate
Prostate brachytherapy - discharge
References
Cooney KA, Heath EI. Prostate cancer. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 186.
National Cancer Institute website. Prostate cancer screening (PDQ) - health professional version. www.cancer.gov/types/prostate/hp/prostate-screening-pdq#section/all. Updated March 7, 2024. Accessed July 16, 2024.
Salami SS, Palapattu GS, Partin AW, Morgan TM. Prostate cancer biomarkers. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 149.
US Preventive Services Task Force; Grossman DC, Curry SJ, et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(18):1901-1913. PMID: 29801017 pubmed.ncbi.nlm.nih.gov/29801017/.
BACK TO TOPReview Date: 1/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Internal review and update on 07/16/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
