Heart bypass surgery
Off-pump coronary artery bypass; OPCAB; Beating heart surgery; Bypass surgery - heart; CABG; Coronary artery bypass graft; Coronary artery bypass surgery; Coronary bypass surgery; Coronary artery disease - CABG; CAD - CABG; Angina - CABG
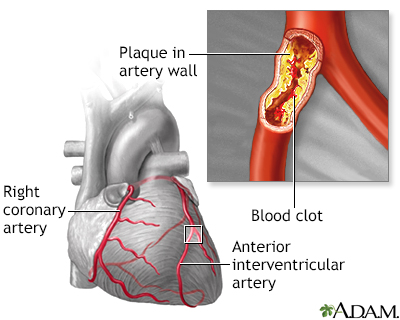
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to go around a blockage to reach your heart.
Images
Presentation

Animation


Description
Before your surgery, you will get general anesthesia. You will be asleep (unconscious) and pain-free during surgery.
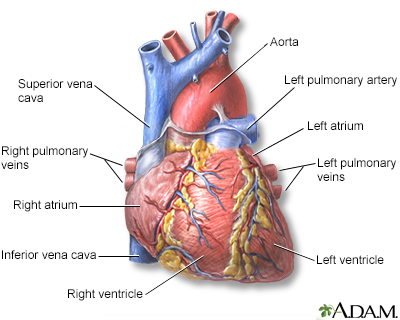
Once you are unconscious, the heart surgeon will make an 8 to 10-inch (20.5 to 25.5 cm) surgical cut in the middle of your chest. Your breastbone will be separated to create an opening. This allows your surgeon to see your heart and aorta, the main blood vessel leading from the heart to the rest of your body.
Most people who have heart bypass surgery are connected to a heart-lung bypass machine or bypass pump.
- Your heart is stopped while you are connected to this machine.
- This machine does the work of your heart and lungs while your heart is stopped for the surgery. The machine adds oxygen to your blood, moves blood through your body, and removes carbon dioxide.
Another type of bypass surgery does not use the heart-lung bypass machine. The procedure is done while your heart is still beating. This is called off-pump coronary artery bypass, or OPCAB.
During bypass surgery:
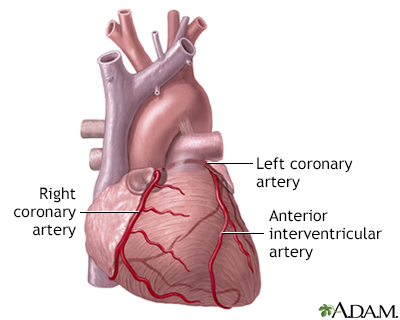
- The surgeon will take a vein or artery from another part of your body and use it to make a detour (or graft) around the blocked area in your artery. Your surgeon may use a vein, called the saphenous vein, from your leg.
- To reach this vein, a surgical cut will be made along the inside of your leg, between your ankle and groin. One end of the graft will be sewn to your coronary artery. The other end will be sewn to an opening made in your aorta.
- A blood vessel in your chest, called the internal mammary artery (IMA), can also be used as the graft. One end of this artery is already connected to a branch of your aorta. The other end is attached to your coronary artery.
- Other arteries can also be used for grafts in bypass surgery. The most common one is the radial artery in your wrist.
After the graft has been created, your breastbone will be closed with wires. These wires stay inside you. The surgical cut will be closed with stitches.
This surgery can take 4 to 6 hours. After the surgery, you will be taken to the intensive care unit.
Why the Procedure Is Performed
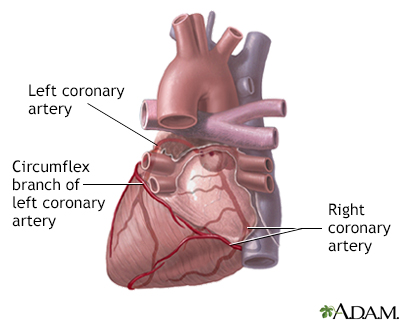
You may need this procedure if you have a blockage in one or more of your coronary arteries. Coronary arteries are the vessels that supply your heart with oxygen and nutrients that are carried in your blood.
When one or more of the coronary arteries becomes partly or totally blocked, your heart does not get enough blood. This is called ischemic heart disease, or coronary artery disease (CAD). It can cause chest pain (angina).
Coronary artery bypass surgery can be used to improve blood flow to your heart. Your health care provider may have first tried to treat you with medicines. You may have also tried exercise and diet changes, or angioplasty with stenting.
CAD is different from person to person. The way it is diagnosed and treated will also vary. Heart bypass surgery is just one type of treatment.
Other procedures that may be used:
Risks
Risks for any surgery include:
- Bleeding
- Infection
- Death
Possible risks from having coronary bypass surgery include:
- Infection, including chest wound infection, which is more likely to happen if you are obese, have diabetes, or have already had this surgery
- Heart attack
- Stroke
- Heart rhythm problems
- Kidney failure
- Lung failure
- Depression and mood swings
- Low fever, tiredness, and chest pain, together called postpericardiotomy syndrome, which can last up to 6 months
- Memory loss, loss of mental clarity, or "fuzzy thinking"
Before the Procedure
Always tell your provider what drugs you are taking, even medicines or herbs you bought without a prescription.
During the days before your surgery:
- For the 1-week period before surgery, you may be asked to stop taking medicines that make it harder for your blood to clot. These might cause increased bleeding during the surgery. They include aspirin, ibuprofen (such as Advil and Motrin), naproxen (such as Aleve and Naprosyn), and other similar medicines. If you are taking clopidogrel (Plavix), talk with your surgeon about when to stop taking it.
- Ask which medicines you should still take on the day of the surgery.
- If you smoke, try to stop. Ask your provider for help.
- Contact your provider if you have a cold, flu, fever, herpes breakout, or any other illness.
- Prepare your home so you can move around easily when you return from the hospital.
The day before your surgery:
- Shower and shampoo well.
- You may be asked to wash your whole body below your neck with a special soap. Scrub your chest 2 or 3 times with this soap.
- Make sure that you dry yourself off.
On the day of the surgery:
- You will be asked not to drink or eat anything after midnight the night before your surgery. Rinse your mouth with water if it feels dry, but be careful not to swallow.
- Take any medicines that you have been told to take with a small sip of water.
You will be told when to arrive at the hospital.
After the Procedure
After the operation, you will spend 3 to 7 days in the hospital. You will spend the first night in an intensive care unit (ICU). You will probably be moved to a regular or transitional care room within 24 to 48 hours after the procedure.
Two to three tubes will be in your chest to drain fluid from around your heart. They are most often removed 1 to 3 days after surgery.
You may have a catheter (flexible tube) in your bladder to drain urine. You may also have intravenous (IV) lines for fluids. You will be attached to machines that monitor your pulse, temperature, and breathing. Nurses will constantly watch your monitors.
You may have several small wires that are connected to a pacemaker, which are pulled out prior to your discharge.
You will be encouraged to restart some activities and you may begin a cardiac rehab program within a few days.
It takes 4 to 6 weeks to start feeling better after surgery. Your providers will tell you how to take care of yourself at home after the surgery.
Outlook (Prognosis)
Recovery from surgery takes time. You may not see the full benefits of your surgery for 3 to 6 months. In most people who have heart bypass surgery, the grafts stay open and work well for many years.
This surgery does not prevent the coronary artery blockage from coming back. You can do many things to slow this process down, including:
- Not smoking
- Eating a heart-healthy diet
- Getting regular exercise
- Treating high blood pressure
- Controlling high blood sugar (diabetes) and high cholesterol
- Taking your medicines as prescribed
Related Information
AtherosclerosisAngina
Heart attack
Angioplasty and stent placement - carotid artery
Heart bypass surgery - minimally invasive
Bathroom safety for adults
Surgical wound care - open
Preventing falls
Angina - when you have chest pain
Angina - discharge
Heart attack – discharge
Aspirin and heart disease
Butter, margarine, and cooking oils
Cholesterol and lifestyle
Antiplatelet medicines - P2Y12 inhibitors
Controlling your high blood pressure
Heart bypass surgery - discharge
Dietary fats explained
Fast food tips
Heart disease - risk factors
How to read food labels
Low-salt diet
Mediterranean diet
When you have nausea and vomiting
Angina - what to ask your doctor
Heart attack - what to ask your provider
Cholesterol - drug treatment
Angioplasty and stent - heart - discharge
Being active after your heart attack
Being active when you have heart disease
Cardiac catheterization - discharge
Heart pacemaker - discharge
References
Doesnt T, Taggart D, Gaudino MFL. Coronary artery bypass grafting. In: Sellke FW, del Nido PJ, Swanson SJ, eds. Sabiston and Spencer Surgery of the Chest. 10th ed. Philadelphia, PA: Elsevier; 2024:chap 91.
Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(3):e18-e114. PMID: 34882435 pubmed.ncbi.nlm.nih.gov/34882435/.
Morrow DA, de Lemos JA. Stable ischemic heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 40.
Omer S, Bakaeen FG. Acquired heart disease: coronary insufficiency. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 60. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 59.
Teirstein PS, Kirtane AJ. Interventional diagnosis and treatment of coronary artery disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine.
BACK TO TOPReview Date: 4/16/2023
Reviewed By: Mary C. Mancini, MD, PhD, Cardiothoracic Surgeon, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Internal review and update on 02/04/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
