Patent ductus arteriosus
PDA
Patent ductus arteriosus (PDA) is a condition in which the ductus arteriosus does not close. The word "patent" means open.
The ductus arteriosus is a blood vessel that allows blood to go around the baby's lungs before birth. Soon after the infant is born and the lungs fill with air, the ductus arteriosus is no longer needed. It most often closes in a couple of days after birth. If the vessel doesn't close, it is referred to as a PDA.
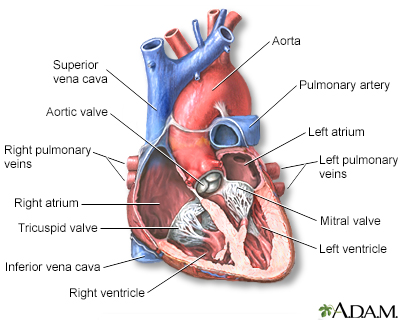
PDA leads to abnormal blood flow between the 2 major blood vessels that carry blood from the heart to the lungs and to the rest of the body.
Images
Presentation

Causes
PDA is more common in girls than boys. The condition is more common in premature infants and those with neonatal respiratory distress syndrome. Infants with genetic disorders, such as Down syndrome, or babies whose mothers had rubella during pregnancy are at higher risk for PDA.
PDA is common in babies with congenital heart problems, such as hypoplastic left heart syndrome, transposition of the great vessels, and pulmonary stenosis.
Symptoms
A small PDA may not cause any symptoms. However, some infants may have symptoms such as:
- Fast breathing
- Poor feeding habits
- Rapid pulse
- Shortness of breath
- Sweating while feeding
- Tiring very easily
- Poor growth
Exams and Tests
Babies with PDA often have a heart murmur that can be heard with a stethoscope. However, in premature infants, a heart murmur may not be heard. The health care provider may suspect the condition if the infant has breathing or feeding problems soon after birth.
Changes may be seen on chest x-rays. The diagnosis is confirmed with an echocardiogram.
Sometimes, a small PDA may not be diagnosed until later in childhood.
Treatment
If there are no other heart defects present, often the goal of treatment is to close the PDA. However, if the baby has certain other heart problems or defects, keeping the ductus arteriosus open may be lifesaving. Medicine may be used to stop it from closing.
Sometimes, a PDA may close on its own. In premature babies, it often closes within the first 2 years of life. In full-term infants, a PDA that remains open after the first several weeks rarely closes on its own.
When treatment is needed, medicines such as indomethacin or ibuprofen are often the first choice. Medicines can work very well for some newborns, with few side effects. The earlier treatment is given, the more likely it is to succeed.
A medication called prostaglandin E1 may be used to keep the PDA open if necessary until other defects are treated.
If these measures do not work or can't be used, the baby may need to have a medical procedure.
A transcatheter device closure is a procedure that uses a thin, hollow tube placed into a blood vessel. The doctor passes a small metal coil or other blocking device through the catheter to the site of the PDA. This blocks blood flow through the vessel. These coils can help the baby avoid surgery.
Surgery may be needed if the catheter procedure does not work or it cannot be used due to the baby's size or other reasons. Surgery involves making a small cut between the ribs to repair the PDA.
Outlook (Prognosis)
If a small PDA stays open, the baby may eventually develop heart symptoms. Babies with a larger PDA could develop heart problems such as heart failure, high blood pressure in the arteries of the lungs, or an infection of the inner lining of the heart if the PDA does not close.
When to Contact a Medical Professional
This condition is most often diagnosed by the provider who examines your infant. Breathing and feeding problems in an infant can sometimes be due to a PDA that has not been diagnosed.
Prevention
Women who plan to become pregnant should be immunized against rubella if they are not already immune. Rubella infection in a pregnant woman can cause congenital heart disease.
Women who are pregnant should get good prenatal care:
- Avoid alcohol and illegal drugs during pregnancy.
- Tell your provider that you are pregnant before taking any new medicines.
- Have a blood test early in your pregnancy to see if you are immune to rubella. If you are not immune, avoid any possible exposure to rubella and get vaccinated right after delivery.
- Pregnant women who have diabetes should try to get good control over their blood sugar level.
Certain genes may play a role in congenital heart disease. Many family members may be affected. Talk to your provider about genetic counseling and screening if you have a family history of congenital heart disease.
Related Information
Premature infantNeonatal respiratory distress syndrome
Heart failure
Pediatric heart surgery
Pediatric heart surgery - discharge
References
Valente AM, Dorfman AL, Babu-Narayan SV, Kreiger EV. Congenital heart disease in the adolescent and adult. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 82.
Well A, Fraser CD. Congenital heart disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 59.
BACK TO TOPReview Date: 10/23/2023
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
