Hydatidiform mole
Hydatid mole; Molar pregnancy; Hyperemesis - molar
Hydatidiform mole (HM) is a rare mass or growth that forms inside the womb (uterus) at the beginning of a pregnancy. It is a type of gestational trophoblastic disease (GTD).
Images
I Would Like to Learn About:
Causes
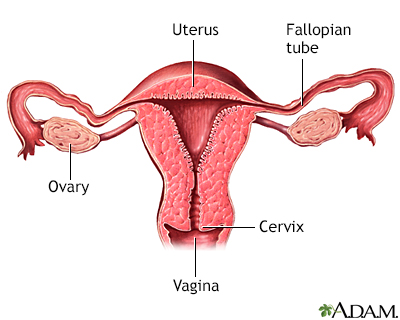
HM, or molar pregnancy, results from abnormal fertilization of the oocyte (egg). It results in an abnormal fetus. The placenta grows normally with little or no growth of the fetal tissue. The placental tissue forms a mass in the uterus. On ultrasound, this mass often has a grape-like appearance, as it contains many small cysts.
The chance of mole formation is higher in older women. A history of mole in earlier years is also a risk factor.
Molar pregnancy can be of two types:
- Partial molar pregnancy: There is an abnormal placenta and some fetal development.
- Complete molar pregnancy: There is an abnormal placenta and no fetus.
There is no way to prevent formation of a molar pregnancy.
Symptoms
Symptoms of a molar pregnancy may include:
- Abnormal growth of the uterus, either bigger or smaller than usual
- Severe nausea and vomiting
- Vaginal bleeding during the first 3 months of pregnancy
- Symptoms of hyperthyroidism, including heat intolerance, loose stools, rapid heart rate, restlessness or nervousness, warm and moist skin, trembling hands, or unexplained weight loss
- Symptoms similar to preeclampsia that occur in the first trimester or early second trimester, including high blood pressure and swelling in the feet, ankles, and legs (this is almost always a sign of a hydatidiform mole, because preeclampsia is extremely rare this early in a normal pregnancy)
Exams and Tests
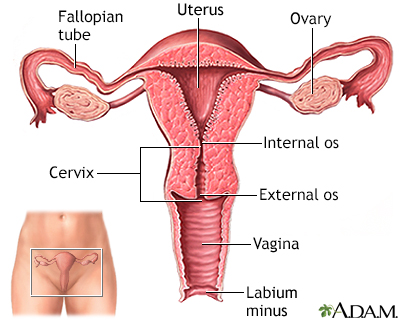
Your health care provider will perform a pelvic exam, which may show signs similar to a normal pregnancy. However, the size of the womb may be abnormal and there may be no heart sounds from the baby. Also, there may be some vaginal bleeding.
A pregnancy ultrasound will show a snowstorm appearance with an abnormal placenta, with or without some development of a baby.
Tests done may include:
- hCG (or HCG, both quantitative) blood test
- Abdominal or vaginal ultrasound of the pelvis
- Chest x-ray
- CT or MRI of the abdomen (imaging tests)
- Complete blood count (CBC)
- Blood clotting tests
- Kidney and liver function tests
Treatment
If your provider suspects a molar pregnancy, removal of the abnormal tissue with a dilation and curettage (D&C) will most likely be suggested. D&C may also be done using suction. This is called suction aspiration (The method uses a suction cup to remove contents from the uterus).
Very rarely, a partial molar pregnancy can continue. A woman may choose to continue her pregnancy in the hope of having a successful birth and delivery. However, these are very high-risk pregnancies. Risks may include bleeding, problems with blood pressure, and premature delivery (having the baby before it is fully developed). In rare cases, the fetus is genetically normal. Women need to completely discuss the risks with their provider before continuing the pregnancy.
A hysterectomy (surgery to remove the uterus) may be an option for older women who do not wish to become pregnant in the future.
After treatment, your hCG level will be followed. It is important to avoid another pregnancy and to use a reliable contraceptive for 6 to 12 months after treatment for a molar pregnancy. This time allows for accurate testing to be sure that the abnormal tissue does not grow back. Women who get pregnant too soon after a molar pregnancy are at high risk of having another molar pregnancy.
Outlook (Prognosis)
Most HMs are noncancerous (benign). Treatment is usually successful. Close follow-up by your provider is important to ensure that signs of the molar pregnancy are gone and pregnancy hormone levels return to normal.
About 15% of cases of HM can become invasive. These moles can grow deep into the uterine wall and cause bleeding or other complications. This type of mole most often responds well to medicines.
In very few cases of complete HM, moles develop into a choriocarcinoma. This is a fast-growing cancer. It is usually successfully treated with chemotherapy, but can be life threatening.
Possible Complications
Complications of molar pregnancy may include:
- Change to invasive molar disease or choriocarcinoma
- Preeclampsia
- Thyroid problems
- Molar pregnancy that continues or comes back
Complications from surgery to remove a molar pregnancy may include:
- Excessive bleeding, possibly requiring a blood transfusion
- Side effects of anesthesia
Related Information
Protein in dietFolic acid in diet
Beta-carotene blood test
References
Nica A, Bouchard-Fortier G, Covens A. Gestational trophoblastic disease: hydatidiform mole, nonmetastatic and metastatic gestational trophoblastic tumor: diagnosis and management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 34.
Soper JT. Gestational trophoblastic disease. In: Creasman WT, Mutch DG, Mannel RS, Tewari KS, eds. DiSaia and Creasman Clinical Gynecologic Oncology. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 7.
Tidy J. Gestational trophoblastic disease. In: Magowan B, ed. Clinical Obstetrics and Gynaecology. 5th ed. Philadelphia, PA: Elsevier Limited; 2023:chap 15.
BACK TO TOPReview Date: 10/15/2024
Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
