Preeclampsia
Toxemia; Pregnancy-induced hypertension (PIH); Gestational hypertension; High blood pressure - preeclampsia
Preeclampsia is high blood pressure and signs of liver or kidney damage that occur in women after the 20th week of pregnancy. While it is rare, preeclampsia also may occur in a woman after delivering her baby, most often within 48 hours. This is called postpartum preeclampsia.
Images
Animation

Causes
The exact cause of preeclampsia is unknown. It occurs in 3% to 7% of all pregnancies. The condition is thought to start in the placenta. Factors that may lead to preeclampsia developing include:
- Autoimmune disorders such as lupus
- Blood vessel problems
- Your diet
- Your genes
Risk factors for the condition include:
- First pregnancy
- Past history of preeclampsia
- Past history of a growth-impaired baby
- Multiple pregnancy (twins or more)
- Family history of preeclampsia
- Obesity
- Being older than age 35
- Being African American
- Being pregnant more than 10 years after a previous pregnancy
- History of diabetes, high blood pressure, or kidney disease
- History of thyroid disease
- IVF pregnancy, especially after a frozen embryo transfer
Symptoms
Often, women who have preeclampsia do not feel sick.
Symptoms of preeclampsia can include:
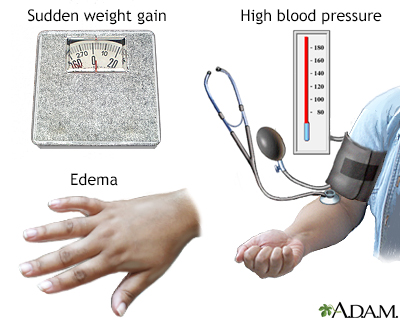
- Swelling of the hands and face or areas around the eyes (periorbital edema)
- Sudden weight gain over 1 to 2 days or more than 2 pounds (0.9 kg) a week
Note: Some swelling of the feet and ankles is considered normal during pregnancy.
Symptoms of severe preeclampsia include:
- Headache that does not go away or becomes worse.
- Trouble breathing.
- Belly pain on the right side, below the ribs. Pain may also be felt in the right shoulder, and can be confused with heartburn, gallbladder pain, a stomach virus, or kicking by the baby.
- Urinating less often than usual.
- Nausea and vomiting (a worrisome sign).
- Vision changes, including temporary blindness, seeing flashing lights or spots, sensitivity to light, and blurry vision.
- Feeling lightheaded or faint.
Exams and Tests
The health care provider will do a physical exam. This may show:
- High blood pressure, often 140/90 mm Hg or higher
- Swelling in the hands and face
- Weight gain
Blood and urine tests will be done. This may show:
- Protein in the urine (proteinuria)
- Higher-than-normal liver enzymes
- Platelet count that is low
- Higher-than-normal creatinine levels in your blood (kidney function test)
- Elevated uric acid levels in your blood
Tests will also be done to:
- See how well your blood clots
- Monitor the baby's health
The results of a pregnancy ultrasound, non-stress test, and other tests will help your provider decide whether your baby needs to be delivered right away.
Women who had low blood pressure at the start of their pregnancy, followed by a significant rise in blood pressure need to be watched closely for other signs of preeclampsia.
Treatment
Preeclampsia usually resolves within 6 weeks after the baby is born and the placenta is delivered. However, it may persist longer or even begin after delivery.
Most often, at 37 weeks, your baby is developed enough to be healthy outside of the womb.
As a result, your provider will likely want your baby to be delivered so the preeclampsia does not get worse. You may get medicines to help trigger labor, or you may need a C-section.
If your baby is not fully developed and you have mild preeclampsia, the disease can often be managed at home until your baby has matured. The provider will recommend:
- Frequent provider visits to make sure you and your baby are doing well.
- Medicines to lower your blood pressure (sometimes).
- The severity of preeclampsia may change quickly, so you'll need very careful follow-up.
Complete bed rest is no longer recommended.
Sometimes, a pregnant woman with preeclampsia is admitted to the hospital. This allows the health care team to monitor the baby and mother more closely.
Treatment in the hospital may include:
- Close monitoring of the mother and baby
- Medicines to control blood pressure and prevent seizures and other complications
- Steroid injections for pregnancies under 34 weeks gestation to help speed up the development of the baby's lungs
You and your provider will continue to discuss the safest time to deliver your baby, considering:
- How close you are to your due date.
- The severity of the preeclampsia. Severe preeclampsia is diagnosed by the level of blood pressure elevation as well as abnormal blood test results as discussed below.
- How well the baby is doing in the womb.
The baby must be delivered if there are signs of severe preeclampsia. These include:
- Tests that show your baby is not growing well or is not getting enough blood and oxygen.
- The bottom number of your blood pressure (diastolic blood pressure) is over 110 mm Hg or is greater than 100 mm Hg consistently over a 24-hour period.
- Abnormal liver function test results.
- Severe headaches.
- Pain in the belly area (abdomen).
- Seizures or changes in mental function (eclampsia).
- Fluid buildup in the mother's lungs.
- HELLP syndrome (rare).
- Low platelet count or bleeding.
- Low urine output, a lot of protein in the urine, and other signs that your kidneys are not working properly.
Outlook (Prognosis)
Signs and symptoms of preeclampsia most often go away within 6 weeks after delivery. However, the high blood pressure sometimes gets worse the first few days after delivery. You are still at risk for preeclampsia for up to 6 weeks after delivery. This postpartum preeclampsia carries a higher risk of death. If you notice any symptoms of preeclampsia, contact your provider right away.
If you have had preeclampsia, you are more likely to develop it again during another pregnancy. In most cases, it is not as severe as the first time.
If you have high blood pressure during more than one pregnancy, you are more likely to have high blood pressure when you get older.
Possible Complications
Rare but severe immediate complications for the mother can include:
- Bleeding problems
- Seizure (eclampsia)
- Fetal growth retardation
- Premature separation of the placenta from the uterus before the baby is born (abruption of the placenta)
- Rupture of the liver
- Stroke
- Death (rarely)
Having a history of preeclampsia makes a woman a higher risk for future problems such as:
- Heart disease
- Diabetes
- Kidney disease
- Chronic high blood pressure
When to Contact a Medical Professional
Contact your provider if you have symptoms of preeclampsia during your pregnancy or after delivery.
Prevention
There is no sure way to prevent preeclampsia.
- If your provider thinks you are at high risk of developing preeclampsia, they may suggest that you start baby aspirin (81 mg) daily late in the first trimester or early in the second trimester of your pregnancy. However, DO NOT start baby aspirin unless you have consulted with your doctor first.
- If your provider thinks your calcium intake is low, they may suggest that you take a calcium supplement daily.
- There are no other specific preventive measures for preeclampsia.
It is important for all pregnant women to start prenatal care early and continue it through the pregnancy and after delivery.
Related Information
Urine protein dipstick testDiabetes
High blood pressure in adults - hypertension
Eclampsia
Premature infant
References
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122-1131. PMID: 24150027 pubmed.ncbi.nlm.nih.gov/24150027/.
Harper LM, Tita A, Karumanchi SA. Pregnancy-related hypertension. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 45.
Sibai BM. Preeclampsia and hypertensive disorders. Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 38.
BACK TO TOPReview Date: 4/16/2024
Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
