Melanoma
Skin cancer - melanoma; Malignant melanoma; Lentigo maligna melanoma; Melanoma in situ; Superficial spreading melanoma; Nodular melanoma; Acral lentiginous melanoma
Melanoma is the most dangerous type of skin cancer. It is also the rarest. It is the leading cause of death from skin disease.
Other common types of skin cancer are squamous cell carcinoma and basal cell carcinoma.
Images






I Would Like to Learn About:
Causes
Melanoma is caused by changes (mutations) in skin cells called melanocytes. These cells make a skin color pigment called melanin. Melanin is responsible for skin and hair color.
Melanoma can appear on normal skin. Sometimes it can develop from moles. Moles that are present at birth may develop into melanomas. Larger moles that are present at birth may be at higher risk for developing melanoma.
There are four major types of melanoma:
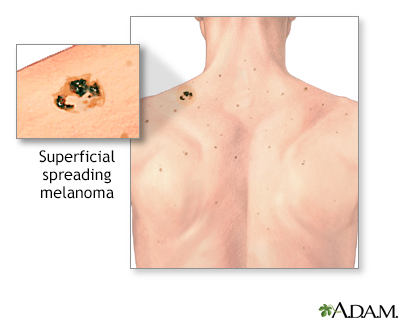
- Superficial spreading melanoma is the most common type. It is usually flat and irregular in shape and color, with different shades of black and brown. It is most common in fair skin people.
- Nodular melanoma usually starts as a raised area that is dark blackish-blue or bluish-red. Some do not have any color (amelanotic melanoma).
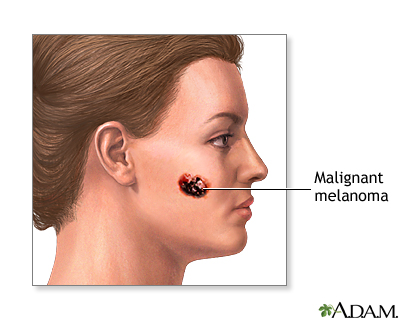
- Lentigo maligna melanoma usually occurs in older people. It is most common in sun-damaged skin on the face, neck, and arms. The abnormal skin areas are usually large, flat, and tan with areas of brown.
- Acral lentiginous melanoma is the least common form. It usually occurs on the palms, soles, or under the nails.
The risk for developing melanoma increases with age. However, more and more young people are developing it.
You are more likely to develop melanoma if you:
- Have fair skin, blue or green eyes, or red or blond hair
- Live in sunny climates or at high altitudes
- Spent a lot of time in high levels of strong sunlight because of a job or other activities
- Have had one or more blistering sunburns during childhood
- Use tanning devices, such as tanning beds
Other risk factors include:
- Having close relatives with melanoma
- Certain types of moles (atypical or dysplastic) or many birthmarks
- Weakened immune system due to disease or medicines
Symptoms
A mole, sore, lump, or growth on the skin can be a sign of melanoma or other skin cancer. A sore or growth that bleeds, or changes in color can also be a sign of skin cancer.
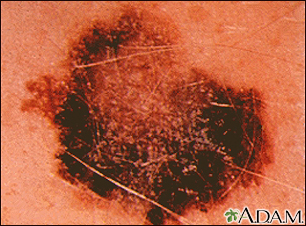
The ABCDE system can help you remember possible symptoms of melanoma:
- Asymmetry: One half of the abnormal area is different from the other half.
- Borders: The edges of the growth are irregular.
- Color: Color changes from one area to another, with shades of tan, brown, or black, and sometimes white, red, or blue. A mixture of colors may appear within one sore.
- Diameter: The spot is usually (but not always) larger than 5 mm in diameter -- about the size of a pencil eraser.
- Evolution: The mole keeps changing appearance.
Another way to look for possible melanoma is the "ugly duckling sign." This means the melanoma does not look like any of the other spots on the body. It stands out like the ugly duckling in the children's story.
Exams and Tests
Your health care provider will check your skin and look at the size, shape, color, and texture of any suspicious areas with a dermatoscope.
If your provider thinks you might have skin cancer, a piece of skin from the growth will be removed. This is called a skin biopsy. The sample is sent to a lab for examination under a microscope.
A sentinel lymph node (SLN) biopsy may be done in some people with melanoma to see if the cancer has spread to nearby lymph nodes.
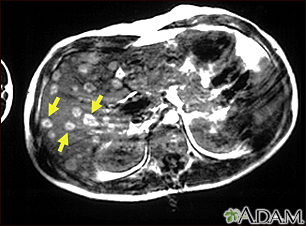
Once melanoma has been diagnosed, CT scans or other types of x-rays may be done to see if the cancer has spread.
Treatment
Surgery is almost always needed to treat melanoma. The skin cancer and some surrounding area will be removed. How much skin is removed depends on how deep the melanoma has grown.
If the cancer has spread to nearby lymph nodes, these lymph nodes may also be removed. After surgery, depending on the risk of the disease returning, you may receive chemotherapy or immunotherapy.
Treatment is more difficult when the melanoma has spread to other organs. Treatment involves shrinking the skin cancer and treating the cancer in other areas of the body. You may receive:
- Chemotherapy: Medicines are used to kill cancer cells directly.
- Immunotherapy: These include medicines such as interferon to help your immune system fight the cancer, or other medicines that boost your immune system's ability to find cancer cells and kill them. They may be used along with chemotherapy and surgery.
- Radiation treatments: These may be used to kill cancer cells.
- Surgery: Surgery may be done to remove cancer that has spread to other parts of the body. This is done to relieve pain or discomfort associated with the growing cancer.
- Topical medicine: It boosts the immune system in local areas.
If you have melanoma that is hard to treat, you might consider enrolling in a clinical trial. Ask your provider for more information. Researchers continue to study new treatments.
Support Groups
Sharing with others who have common experiences and problems can help you not feel alone. More information and support for people with melanoma and their families can be found at:
- National Cancer Institute -- www.cancer.gov/about-cancer/coping/adjusting-to-cancer/support-groups
- American Cancer society -- www.cancer.org/cancer/melanoma-skin-cancer
- The American Melanoma Foundation -- melanomafoundation.org/
Outlook (Prognosis)
How well you do depends on many things, including how early the cancer was diagnosed, and how far it has spread.
In its early stage, most melanomas can be cured by surgery.
Melanoma that is very deep or has spread to the lymph nodes is more likely to return after treatment. If it is deeper than 4 mm or has spread to the lymph nodes, the cancer is more likely to have spread to other tissues and organs.
If you have had melanoma and recovered, it is very important to examine your body regularly for any unusual changes. Your risk for melanoma increases once you have had this cancer. Melanoma can return years later.
Possible Complications
Melanoma can spread to other parts of the body.
Melanoma treatment can cause side effects, including pain, nausea, and fatigue.
When to Contact a Medical Professional
Contact your provider if you notice a new growth or any other changes in your skin. Also talk to your provider if an existing spot:
- Changes in shape, size or color
- Become painful, swollen, or inflamed
- Starts to bleed or itch
Prevention
Some people should see a skin specialist (dermatologist) for regular skin exams. These include people with:
- A family history of melanoma
- Severely sun-damaged skin
- Lots of moles on their skin
A skin specialist can examine you and tell you whether you need regular skin checks. Sometimes, unusual moles are removed to prevent them from turning into melanoma.
You should also examine your own skin once a month. Use a mirror to check hard-to-see places. Use the ABCDE system and the "ugly duckling" sign when checking your skin.
The best way to prevent skin cancer is to reduce your exposure to sunlight. Ultraviolet light is most intense between 10 a.m. and 4 p.m. Try to avoid sun exposure during these hours. Protect your skin by wearing a hat, long-sleeved shirt, long skirt, or pants when you have to be outside. The following tips can also help:
- Apply high-quality sunscreen with a sun protection factor (SPF) rating of 30 or higher, even when you are only going outdoors for a short time.
- Apply a large amount of sunscreen on all exposed areas, including ears and feet.
- Look for sunscreens that block both UVA and UVB light. These will have the label "broad spectrum."
- Use a waterproof formula if exposed to water.
- Apply sunscreen at least 30 minutes before going outside. Reapply it often, especially after swimming.
- Use sunscreen in winter, too. Protect yourself even on cloudy days.
Other important facts to help you avoid too much sun exposure:
- Avoid surfaces that reflect more light, such as water, sand, concrete, and white-painted areas.
- Be extra careful at higher altitudes, where skin burns faster.
- Avoid sun lamps, tanning beds, and tanning salons.
Even though melanoma can develop in some moles, dermatologists feel that there is no advantage to remove moles to prevent melanoma.
Related Information
Melanoma of the eyeReferences
National Cancer Institute website. Melanoma treatment (PDQ) health professional version. www.cancer.gov/types/skin/hp/melanoma-treatment-pdq. Updated April 16, 2024. Accessed April 22, 2024.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology: melanoma: cutaneous version 2. 2024. www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf. Updated April 3, 2024. Accessed April 22, 2024.
North JP, Bastian BC, Lazar AJ. Melanoma. In: Calonje E, Bren T, Lazar AJ, Billings SD, eds. McKee's Pathology of the Skin. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 26.
Zaba LC, Wang JY, Swetter SM. Melanoma. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 113.
BACK TO TOPReview Date: 2/15/2024
Reviewed By: Elika Hoss, MD, Assistant Professor of Dermatology, Mayo Clinic, Scottsdale, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
