Duchenne muscular dystrophy
Pseudohypertrophic muscular dystrophy; Muscular dystrophy - Duchenne type
Duchenne muscular dystrophy is an inherited disorder. It involves muscle weakness, which quickly gets worse.
Images
Causes
Duchenne muscular dystrophy is a form of muscular dystrophy. It worsens quickly. Other muscular dystrophies (including Becker muscular dystrophy) get worse much more slowly.
Duchenne muscular dystrophy is caused by a defective gene for dystrophin (a protein in the muscles). However, it often occurs in people without a known family history of the condition.
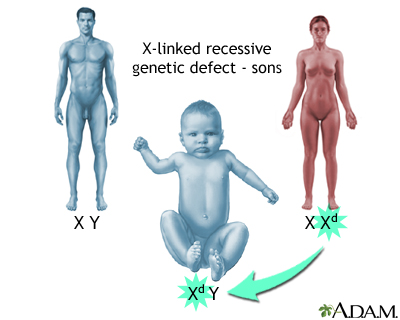
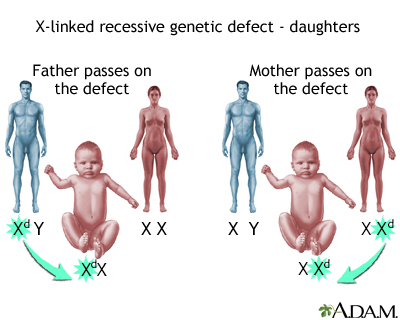
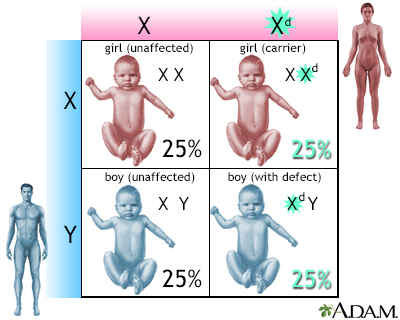
The condition most often affects boys due to the way the disease is inherited. The sons of women who are carriers of the disease (women with a defective gene, but no symptoms themselves) each have a 50% chance of having the disease. The daughters each have a 50% chance of being carriers. Very rarely, a female can be affected by the disease.
Duchenne muscular dystrophy occurs in about 1 out of every 3,600 male infants. Because this is an inherited disorder, risks include a family history of Duchenne muscular dystrophy.
Symptoms
Symptoms most often appear before age 6. They may start as early as infancy. Most boys show no symptoms in the first few years of life.
Symptoms may include:
- Fatigue
- Learning difficulties (the IQ can be below 75).
- Intellectual disability (possible, but does not get worse over time).
Muscle weakness:
- Begins in the legs and pelvis, but also occurs less severely in the arms, neck, and other areas of the body.
- Problems with motor skills (running, hopping, jumping).
- Frequent falls.
- Trouble getting up from a lying position or climbing stairs.
- Shortness of breath, fatigue, and swelling of the feet due to a weakening of the heart muscle.
- Problem breathing due to a weakening of the respiratory muscles.
- Gradual worsening of muscle weakness.
Progressive difficulty walking:
- Ability to walk may be lost by age 12, and the child will have to use a wheelchair.
- Breathing difficulties and heart disease usually start by age 20.
Exams and Tests
A complete nervous system (neurological), heart, lung, and muscle exam may show:
- Abnormal, weak heart muscle (cardiomyopathy) that becomes evident by age 10
- Congestive heart failure or irregular heart rhythm (arrhythmias) that is present in all people with Duchenne muscular dystrophy by the age of 18
- Deformities of the chest and back (scoliosis)
- Enlarged muscles of the calves, buttocks, and shoulders (around age 4 or 5). These muscles are eventually replaced by fat and connective tissue (pseudohypertrophy).
- Loss of muscle mass (wasting)
- Muscle contractures in the heels, legs
- Muscle deformities
- Respiratory disorders, including pneumonia and swallowing with food or fluid passing into the lungs (in late stages of the disease)
Tests may include:
- Blood creatine kinase levels
- Electrocardiogram (ECG)
- Cardiac testing
- X-rays of the spine to determine if there is a scoliosis
- Pulmonary function tests
- Electromyography (EMG)
- Genetic tests
- Muscle biopsy
Treatment
There is no known cure for Duchenne muscular dystrophy. Treatment aims to control symptoms to improve quality of life.
Steroid drugs can slow the loss of muscle strength. They may be started when the child is diagnosed or when muscle strength begins to decline.
Other treatments may include:
- Albuterol (to help with muscle strength)
- Amino acids
- Carnitine
- Coenzyme Q10
- Creatine
- Fish oil
- Green tea extracts
- Vitamin E
However, the effects of these treatments have not been proven. Stem cells and gene therapy may be used in the future.
Genetic therapies may be helpful to certain patients, depending on the genetic cause. Each therapy only works on a small number of patients, depending on their specific genetic change (mutation). While these treatments have been shown to increase dystrophin production, they have not yet been shown to have significant clinical benefits. Treatments include:
- Eteplirsen
- Golodirsen
- Vitolarsen
- Casimersen
- Ataluren
- Delandistrogene moxeparvovec
The use of steroids and the lack of physical activity can lead to excessive weight gain. Activity is encouraged. Inactivity (such as bedrest) can make the muscle disease worse. Physical therapy may help to maintain muscle strength and function. Speech therapy is often needed.
Other treatments may include:
- Assisted ventilation (used during the day or night)
- Drugs to help heart function, such as angiotensin-converting-enzyme inhibitors, beta-blockers, and diuretics
- Orthopedic appliances (such as braces and wheelchairs) to improve mobility
- Spine surgery to treat progressive scoliosis for some people
- Proton pump inhibitors (for people with gastroesophageal reflux)
Several new treatments are being studied in trials.
Support Groups
You can ease the stress of illness by joining a support group where members share common experiences and problems. The Muscular Dystrophy Association is an excellent source of information on this disease.
Outlook (Prognosis)
Duchenne muscular dystrophy leads to progressively worsening disability. Death often occurs from lung disorders, although advances in supportive care have resulted in many men living to age 35 years.
Possible Complications
Complications may include:
- Cardiomyopathy
- Congestive heart failure (rare)
- Deformities
- Heart arrhythmias (rare)
- Mental impairment (varies, usually minimal)
- Permanent, progressive disability, including decreased mobility and decreased ability to care for self
- Pneumonia or other respiratory infections
- Respiratory failure
When to Contact a Medical Professional
Contact your health care provider if:
- Your child has symptoms of Duchenne muscular dystrophy
- Symptoms get worse, or new symptoms develop, particularly fever with cough or breathing problems
Prevention
People with a family history of the disease may want to seek genetic counseling. Genetic studies done during pregnancy are very accurate in detecting Duchenne muscular dystrophy.
Related Information
WeaknessMuscular dystrophy
Protein in diet
Muscle atrophy
Muscle cramps
Cardiomyopathy
Becker muscular dystrophy
References
Bharucha-Goebel DX. Muscular dystrophies. In: Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 627.
Genetic and Rare Diseases Information Center (GARD). Duchenne muscular dystrophy. rarediseases.info.nih.gov/diseases/6291/duchenne-muscular-dystrophy. Updated June 2024. Accessed June 11, 2024.
Lee BH. The Dystrophinopathies. Continuum (Minneap Minn). 2022;28(6):1678-1697. PMID: 36537975 pubmed.ncbi.nlm.nih.gov/36537975/.
Muscular Dystrophy Association website. Duchenne muscular dystrophy. www.mda.org/disease/duchenne-muscular-dystrophy. Accessed March 5, 2024.
Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389.
Warner WC, Sawyer JR. Neuromuscular disorders. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 35.
BACK TO TOPReview Date: 12/31/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 06/11/2024.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
