Hereditary elliptocytosis
Elliptocytosis - hereditary
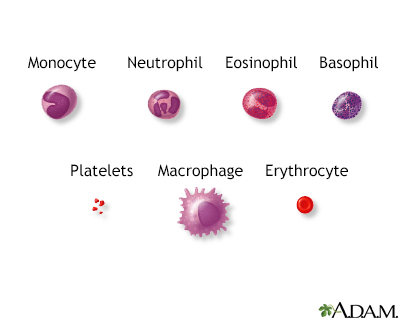
Hereditary elliptocytosis is a disorder passed down through families in which the red blood cells are abnormally shaped. It is similar to other blood conditions such as hereditary spherocytosis and hereditary ovalocytosis.
Images

Causes
Elliptocytosis affects about 1 in every 2,500 people of northern European heritage. It is more common in people of African and Mediterranean descent. You are more likely to develop this condition if someone in your family has had it.
Symptoms
Symptoms may include:
- Fatigue.
- Shortness of breath.
- Yellow skin and eyes (jaundice). This may continue for a long time in a newborn.
Exams and Tests
An exam by your health care provider may show an enlarged spleen.
The following test results may help diagnose the condition:
- Bilirubin level may be high.
- Blood smear may show elliptical red blood cells.
- Complete blood count (CBC) may show anemia or signs of red blood cell destruction.
- Lactate dehydrogenase level may be high.
- Imaging of the gallbladder may show gallstones.
Treatment
There is no treatment needed for the disorder unless severe anemia or anemia symptoms occur. Surgery to remove the spleen may decrease the rate of red blood cell damage.
Outlook (Prognosis)
Most people with hereditary elliptocytosis have no problems. They often do not know they have the condition.
Possible Complications
Elliptocytosis is often harmless. In mild cases, fewer than 15% of red blood cells are elliptical-shaped. However, some people may have crises in which the red blood cells rupture. This is more likely to happen when they have a viral infection. People with this disease can develop anemia, jaundice, and gallstones.
When to Contact a Medical Professional
Contact your provider if you have jaundice that does not go away or symptoms of anemia or gallstones.
Prevention
Genetic counseling may be appropriate for people with a family history of this disease who wish to become parents.
Related Information
Autosomal dominantHemoglobin
Anemia
Gallstones
References
Gallagher PG. Hemolytic anemias: red blood cell membrane and metabolic defects. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 147.
Gallagher PG. Red blood cell membrane disorders. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 46.
Prozora S, Gallagher PG. Hereditary elliptocytosis, hereditary pyropoikilocytosis, and related disorders. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 508.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
