Glomerulonephritis
Glomerulonephritis - chronic; Chronic nephritis; Glomerular disease; Necrotizing glomerulonephritis; Glomerulonephritis - crescentic; Crescentic glomerulonephritis; Rapidly progressive glomerulonephritis
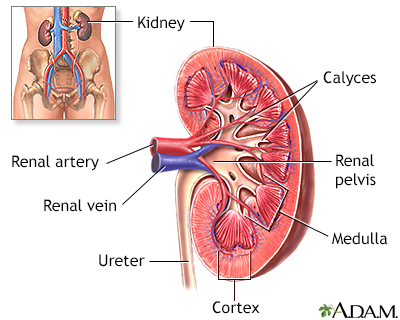
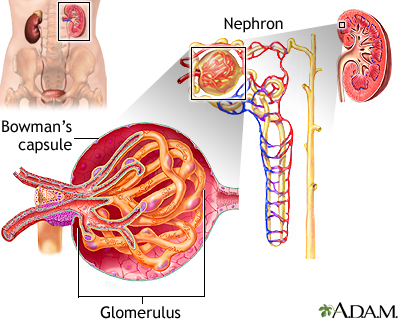
Glomerulonephritis is a type of kidney disease in which the part of your kidneys that helps filter waste and fluids from the blood is damaged.
Images
I Would Like to Learn About:
Causes
The filtering unit of the kidney is called the glomerulus. Each kidney has many thousands of glomeruli. The glomeruli help the body get rid of harmful substances.
Glomerulonephritis may be caused by problems with the body's immune system. Often, the exact cause of this condition is unknown.
Damage to the glomeruli causes blood and protein to be lost in the urine.
The condition may develop quickly, and kidney function is lost within weeks or months. This is called rapidly progressive glomerulonephritis.
Some people with chronic glomerulonephritis have no history of kidney disease.
The following may increase your risk for this condition:
- Blood or lymphatic system disorders
- Exposure to hydrocarbon solvents
- History of cancer
- Infections such as strep infections, viruses, heart infections, or abscesses
Many conditions cause or increase the risk for glomerulonephritis, including:
- Amyloidosis (disorder in which a protein called amyloid builds up in the organs and tissues)
- Disorder that affects the glomerular basement membrane, the part of the kidney that helps filter waste and extra fluid from the blood
- Blood vessel diseases, such as vasculitis or polyarteritis
- Focal segmental glomerulosclerosis (scarring of the glomeruli)
- Anti-glomerular basement membrane disease (disorder in which the immune system attacks the glomeruli)
- Analgesic nephropathy syndrome (kidney disease due to heavy use of pain relievers, especially NSAIDs)
- Henoch-Schönlein purpura (disease that involves purple spots on the skin, joint pain, gastrointestinal problems and glomerulonephritis)
- IgA nephropathy (disorder in which antibodies called IgA build up in kidney tissue)
- Lupus nephritis (kidney complication of systemic lupus erythematosus)
- Membranoproliferative GN (form of glomerulonephritis due to abnormal buildup of antibodies in the kidneys)
Symptoms
Common symptoms of glomerulonephritis are:
- Blood in the urine (dark, rust-colored, or brown urine)
- Foamy urine (due to excess protein in the urine)
- Swelling (edema) of the face, eyes, ankles, feet, legs, or abdomen
Symptoms may also include the following:
- Abdominal pain
- Blood in the vomit or stools
- Cough and shortness of breath
- Diarrhea
- Excessive urination
- Fever
- General ill feeling, fatigue, and loss of appetite
- Joint or muscle aches
- Nosebleed
The symptoms of chronic kidney disease may develop over time.
Chronic kidney failure symptoms may gradually develop.
Exams and Tests
Because symptoms may develop slowly, the disorder may be discovered when you have an abnormal urinalysis during a routine physical or examination for another condition.
Signs of glomerulonephritis can include:
- Anemia
- High blood pressure
- Signs of reduced kidney function
A kidney biopsy confirms the diagnosis.
Later, signs of chronic kidney disease may be seen, including:
- Nerve inflammation (polyneuropathy)
- Signs of fluid overload, including abnormal heart and lung sounds
- Swelling (edema)
Imaging tests that may be done include:
- Abdominal CT scan
- Kidney ultrasound
- Chest x-ray
- Intravenous pyelogram (IVP)
Urinalysis and other urine tests include:
- Creatinine clearance
- Examination of the urine under a microscope
- Uric acid in the urine
- Urine concentration test
- Urine creatinine
- Urine protein
- Urine RBC
- Urine specific gravity
- Urine osmolality
This disease may also cause abnormal results on the following blood tests:
- Albumin
- Antiglomerular basement membrane antibody test
- Antineutrophil cytoplasmic antibodies (ANCAs)
- Antinuclear antibodies
- BUN and creatinine
- Complement levels
- Uric acid
Treatment
Treatment depends on the cause of the disorder, and the type and severity of symptoms. Controlling high blood pressure is usually an important part of treatment.
Medicines that may be prescribed include:
- Blood pressure drugs, most often angiotensin-converting enzyme inhibitors (ACE inhibitors) and angiotensin receptor blockers (ARBs)
- Corticosteroids
- Drugs that suppress the immune system
A procedure called plasmapheresis may sometimes be used for glomerulonephritis caused by immune system problems. The fluid part of the blood that contains antibodies is removed and replaced with intravenous fluids or donated plasma (that does not contain antibodies). Removing antibodies may reduce inflammation in the kidney tissues.
You may need to limit your intake of sodium, fluids, protein, and other substances.
People with this condition should be closely watched for signs of kidney failure. Dialysis or a kidney transplant may eventually be needed.
Support Groups
More information and support for people with glomerulonephritis and their families can be found at kidney disease support group.
Outlook (Prognosis)
Glomerulonephritis may be temporary and reversible, or it may get worse. Progressive glomerulonephritis may lead to:
- Chronic kidney failure
- Reduced kidney function
- End-stage kidney disease
If you have nephrotic syndrome and it can be controlled, you may also be able to control other symptoms. If it cannot be controlled, you may develop end-stage kidney disease.
When to Contact a Medical Professional
Contact your health care provider if:
- You have a condition that increases your risk for glomerulonephritis
- You develop symptoms of glomerulonephritis
Prevention
Most cases of glomerulonephritis can't be prevented. Some cases may be prevented by avoiding or limiting exposure to organic solvents, mercury, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Related Information
UrinalysisHigh blood pressure in adults - hypertension
Acute
Focal segmental glomerulosclerosis
Anti-glomerular basement membrane disease
IgA nephropathy
Lupus nephritis
Membranoproliferative glomerulonephritis
Poststreptococcal glomerulonephritis (GN)
Nephrotic syndrome
Acute nephritic syndrome
Chronic kidney disease
End-stage kidney disease
Malignant hypertension
Heart failure
Pulmonary edema
Urinary tract infection - children
References
Radhakrishnan J, Stokes MB. Glomerular disorders and nephrotic syndromes. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 107.
Radhakrishnan J, Appel GB, D'Agati VD. Secondary glomerular disease. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 32.
Reich HN, Cattran DC. Treatment of glomerulonephritis. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 33.
Saha MK, Pendergraft WF, Jennette JC, Falk RJ. Primary glomerular disease. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 31.
BACK TO TOPReview Date: 8/28/2023
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
