Pericarditis
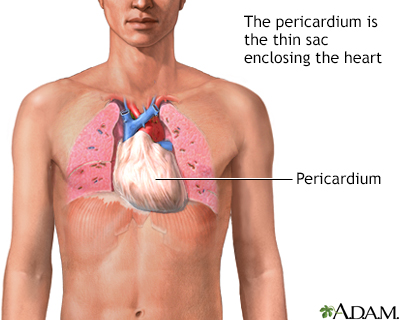
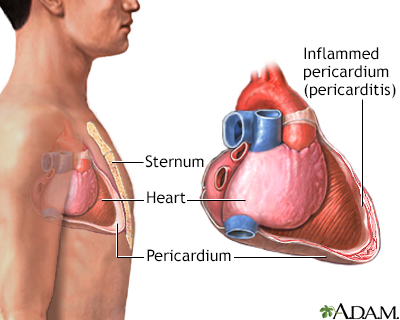
Pericarditis is a condition in which the sac-like covering around the heart (pericardium) becomes inflamed.
Images
I Would Like to Learn About:
Causes
The cause of pericarditis is unknown or unproven in many cases. It mostly affects men ages 20 to 50 years.
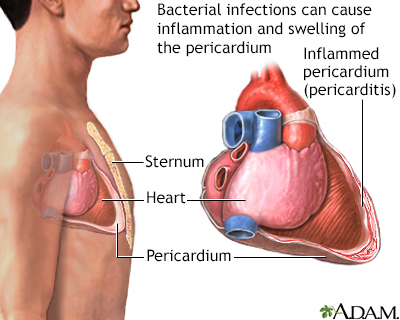
Pericarditis is often the result of an infection such as:
- Viral infections that cause a chest cold or pneumonia
- Infections with bacteria (less common)
- Some fungal infections (rare)
The condition may be seen with diseases such as:
- Cancer (including leukemia)
- Disorders in which the immune system attacks healthy body tissue by mistake (autoimmune diseases)
- HIV infection and AIDS
- Underactive thyroid gland
- Kidney failure
- Rheumatic fever
- Tuberculosis (TB)
Other causes include:
- Heart attack
- Heart surgery or trauma to the chest, esophagus, or heart
- Certain medicines, such as procainamide, hydralazine, phenytoin, isoniazid, and some drugs used to treat cancer or suppress the immune system
- Swelling or inflammation of the heart muscle (myocarditis)
- Radiation therapy to the chest
Symptoms
Chest pain is almost always present. The pain:
- May be felt in the neck, shoulder, back, or abdomen
- Often increases with deep breathing and lying flat, and may increase with coughing and swallowing
- Can feel sharp and stabbing
- Is often relieved by sitting up and leaning or bending forward
You may have fever, chills, or sweating if the condition is caused by an infection.
Other symptoms may include:
Exams and Tests
When listening to the heart with a stethoscope, the health care provider can hear a sound called a pericardial rub. The heart sounds may be muffled or distant. There may be other signs of excess fluid in the pericardium (pericardial effusion).
If the disorder is severe, there may be:
- Crackles in the lungs
- Decreased breath sounds
- Other signs of fluid in the space around the lungs
The following imaging tests may be done to check the heart and the tissue layer around it (pericardium):
- Chest MRI scan
- Chest x-ray
- Echocardiogram
- Electrocardiogram (ECG)
- Heart MRI or heart CT scan
- Radionuclide scanning
To look for heart muscle damage, the provider may order a troponin I test. Other laboratory tests may include:
- Antinuclear antibody (ANA)
- Blood culture
- CBC
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- HIV test
- Rheumatoid factor
- Tuberculin skin test
Treatment
The cause of pericarditis should be identified, if possible.
High doses of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or indomethacin are often given with a medicine called colchicine. These medicines will decrease your pain and reduce the swelling or inflammation in the sac around your heart. You will be asked to take them for days to weeks or longer in some cases.
If the cause of pericarditis is an infection:
- Antibiotics will be used for bacterial infections
- Antifungal medicines will be used for fungal pericarditis
Other medicines that may be used are:
- Corticosteroids such as prednisone (in some people)
- "Water pills" (diuretics) to remove excess fluid
- Other anti-inflammatory agents
If the buildup of fluid makes the heart function poorly, treatment may include:
- Draining the fluid from the sac. This procedure, called pericardiocentesis, is done using a needle, which is guided by ultrasound (echocardiography) in most cases.
- Cutting a small hole (window) in the pericardium (subxiphoid pericardiotomy) to allow the infected fluid to drain into the abdominal cavity. This is done by a surgeon.
Surgery called pericardiectomy may be needed if the pericarditis is long-lasting, comes back after treatment, or causes scarring or tightening of the tissue around the heart. The operation involves cutting or removing part of the pericardium.
Outlook (Prognosis)
Pericarditis can range from mild illness that gets better on its own, to a life-threatening condition. Fluid buildup around the heart and poor heart function can complicate the disorder.
The outcome is good if pericarditis is treated right away. Most people recover in 2 weeks to 3 months. However, pericarditis may come back. This is called recurrent, or chronic, if symptoms or episodes continue.
Scarring and thickening of the sac-like covering and the heart muscle may occur when the problem is severe. This is called constrictive pericarditis. It can cause long-term problems similar to those of heart failure.
When to Contact a Medical Professional
Contact your provider if you have symptoms of pericarditis. This disorder is not life threatening most of the time. However, it can be very dangerous if not treated.
Prevention
Many cases cannot be prevented.
Related Information
SystemicAutoimmune disorders
Rheumatic fever
Pulmonary tuberculosis
Acute kidney failure
HIV/AIDS
Pericarditis - after heart attack
Myocarditis
Respiratory
Arrhythmias
Heart failure
Restrictive cardiomyopathy
References
Azarbal A, LeWinter MM. Pericarditis. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:148-152.
Chabrando JG, Bonaventura A, Vecchie A, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(1):76-92. PMID: 31918837 pubmed.ncbi.nlm.nih.gov/31918837/.
Knowlton KU, Savoia MC, Oxman MN. Myocarditis and pericarditis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 80.
Lewinter MM, Cremer PC, Klein AL. Pericardial diseases. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 86.
BACK TO TOPReview Date: 2/27/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
