Pulmonary embolus
Venous thromboembolism; Lung blood clot; Blood clot - lung; Embolus; Tumor embolus; Embolism - pulmonary; DVT - pulmonary embolism; Thrombosis - pulmonary embolism; Pulmonary thromboembolism; PE
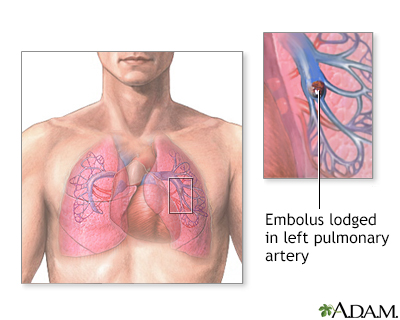
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.
Images
I Would Like to Learn About:
Causes
A pulmonary embolus is most often caused by a blood clot that develops in a vein outside the lungs. The most common blood clot is one in a deep vein of the thigh or in the pelvis (hip area). This type of clot is called a deep vein thrombosis (DVT). The blood clot breaks off and travels to the lungs where it lodges.
Less common causes of a pulmonary embolus include air bubbles, fat droplets, amniotic fluid, or clumps of parasites or tumor cells.
You are more likely to get a pulmonary embolus if you or your family has a history of blood clots or certain clotting disorders. A pulmonary embolus may occur:
- After childbirth
- During a hospital stay when you may be at bedrest or immobilized
- After severe injuries, burns, or fractures of the hips or thigh bone
- After surgery, most commonly bone, joint, or brain surgery
- During or after a long plane or car ride
- If you have cancer
- If you take birth control pills or estrogen therapy
- Long-term bed rest or staying in one position for a long time
Disorders that may lead to blood clots include:
- Diseases of the immune system that make it harder for the blood to clot.
- Inherited disorders that make the blood more likely to clot. One such disorder is antithrombin III deficiency.
Symptoms
The main symptoms of a pulmonary embolism include chest pain that may be any of the following:
- Under the breastbone or on one side
- Sharp or stabbing
- Burning, aching, or a dull, heavy sensation
- Often gets worse with deep breathing
- You may bend over or hold your chest in response to the pain
Other symptoms may include:
- Dizziness, lightheadedness, or fainting
- Low oxygen level in blood (hypoxemia)
- Fast breathing or wheezing
- Fast heart rate
- Feeling anxious
- Leg pain, redness, or swelling
- Low blood pressure
- Sudden cough, possibly coughing up blood or bloody mucus
- Shortness of breath that starts suddenly during sleep or on exertion
- Low grade fever
- Bluish skin (cyanosis) -- less common
Exams and Tests
Your health care provider will perform a physical exam and ask about your symptoms and medical history.
The following lab tests may be done to see how well your lungs are working:
- Arterial blood gases
- Pulse oximetry
The following imaging tests can help determine where the blood clot is located:
- CT angiogram of the chest
- Pulmonary ventilation/perfusion scan, also called a V/Q scan
Other tests that may be done include:
Blood tests may be done to check if you have an increased chance of blood clotting, including:
- Antiphospholipid antibodies
- Antithrombin III level
- Genetic testing to look for changes that make you more likely to develop blood clots
- Lupus anticoagulant
- Protein C and protein S levels
Treatment
A pulmonary embolus requires treatment right away. You may need to stay in the hospital:
- You will receive medicines to thin the blood and make it less likely your blood will form more clots.
- In cases of severe, life-threatening pulmonary embolism, treatment may involve dissolving or removing the clot. This is called thrombolytic therapy or a thrombectomy. You will receive medicines to dissolve the clot.
Whether or not you need to stay in the hospital, you will likely need to take medicines at home to thin the blood:
- You may be given pills to take or you may need to give yourself injections.
- For some medicines, you will need blood tests to monitor your dosage.
- How long you need to take these medicines depends mostly on the cause of your blood clot.
- Your provider will talk to you about the risk of bleeding problems when you take these medicines.
If you cannot take blood thinners, your provider may suggest surgery to place a device called an inferior vena cava filter (IVC filter). This device is placed in the main vein in your belly. It keeps large clots from traveling into the blood vessels of the lungs. Sometimes, a temporary filter can be placed and removed later.
Outlook (Prognosis)
How well a person recovers from a pulmonary embolus can be hard to predict. It depends on:
- What caused the problem in the first place (for example, cancer, major surgery, or an injury)
- The size of the blood clot in the lungs
- If the blood clot dissolves over time
- The person's overall health status
- Some people can develop long-term heart and lung problems.
Death is possible in people with a severe pulmonary embolism.
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number, if you have symptoms of pulmonary embolus.
Prevention
Blood thinners may be prescribed to help prevent DVT in people at high risk, or those who are undergoing high-risk surgery.
If you had a DVT, your provider will prescribe pressure stockings. Wear them as instructed. They will improve blood flow in your legs and reduce your risk for blood clots.
Moving your legs often during long plane trips, car trips, and other situations in which you are sitting or lying down for long periods can also help prevent DVT. People at very high risk for blood clots may need shots of a blood thinner called heparin or other medicine when they take a flight that lasts longer than 4 hours.
Do not smoke. If you smoke, quit. Women who are taking estrogen must stop smoking. Smoking increases your risk of developing blood clots.
Related Information
Deep vein thrombosisCancer
Stroke
Heart attack
Broken bone
Pulmonary hypertension
Taking warfarin (Coumadin, Jantoven) - what to ask your doctor
Taking warfarin
Deep vein thrombosis - discharge
References
Davidson BL, Elliott CG. Pulmonary thromboembolism: prophylaxis and treatment. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 82.
Goldhaber SZ, Piazza G. Pulmonary embolism and deep vein thrombosis. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 87.
Kabrhel C. Pulmonary embolism and deep vein thrombosis. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 74.
Morris TA, Rose A. Pulmonary thromboembolism: presentation and diagnosis. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 81.
Weitz JI, Eikelboom JW. Venous thrombosis and embolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 68.
BACK TO TOPReview Date: 12/31/2023
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
