Angioplasty and stent - heart - discharge
Drug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation - discharge; Angina angioplasty - discharge; Heart attack angioplasty - discharge; CAD angioplasty - discharge
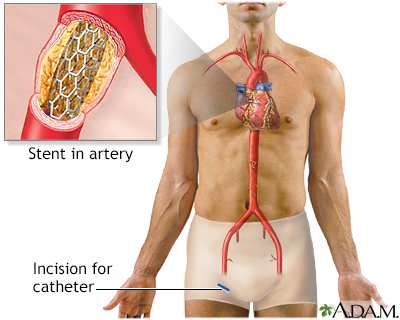
Angioplasty is a procedure to open narrowed or blocked blood vessels, including those that supply blood to the heart. These blood vessels are called the coronary arteries. A coronary artery stent is a small, metal mesh tube that expands inside a coronary artery.
Images
Animation


I Would Like to Learn About:
When You're in the Hospital
You had angioplasty when you were in the hospital. You may have also had a stent placed. Both of these were done to open narrowed or blocked coronary arteries, the blood vessels that supply blood to your heart. You may have had a heart attack or angina (chest pain) before the procedure.
What to Expect at Home
You may have pain in your groin area, arm, or wrist. This is from the catheter (flexible tube) that was inserted to do the procedure. You may also have some bruising around and below the incision.
The chest pain and shortness of breath you likely had before the procedure should be much better now.
Self-care
In general, people who have angioplasty can walk around within 6 hours after the procedure. You may be able to be up and walking earlier if the procedure was performed through the wrist. Complete recovery takes a week or less. Keep the area where the catheter was inserted dry for 24 to 48 hours.
If the provider put the catheter in through your groin:
- Walking short distances on a flat surface is OK. Limit going up and down stairs to around 2 times a day for the first 2 to 3 days.
- Don't do yard work, drive, squat, carry heavy objects, or play sports for at least 2 days, or until your health care provider tells you it is safe.
If the provider put the catheter in your arm or wrist:
- Don't lift anything heavier than 10 pounds (4.5 kilograms) (a little more than a gallon of milk) with the arm that had the catheter.
- Don't do any heavy pushing, pulling, or twisting with that arm.
For a catheter in your groin, arm, or wrist:
- Avoid sexual activity for 2 to 5 days. Ask your provider when it will be OK to start again.
- Don't take a bath or swim for the first week. You may take showers, but make sure the area where the catheter was inserted does not get wet for the first 24 to 48 hours.
- You should be able to return to work in 2 to 3 days if you do not do heavy work.
You will need to care for your incision.
- Your provider will tell you how often to change your dressing.
- If your incision bleeds or swells up, lie down and put pressure on it for 30 minutes.
Angioplasty does not cure the cause of the blockage in your arteries. Your arteries may become narrow again. Eat a heart-healthy diet, exercise, stop smoking (if you smoke), and reduce stress to help lower your chances of having a blocked artery again. Your provider may give you medicine to help lower your cholesterol.
Most people take aspirin together with another antiplatelet medicine such as clopidogrel (Plavix), prasugrel (Efient), or ticagrelor (Brilinta) after this procedure. These medicines are blood thinners. They keep your blood from forming clots in your arteries and stent. A blood clot can lead to a heart attack. Take the medicines exactly as your provider tells you. Do not stop taking them without talking with your provider first.
You should know how to take care of your angina if it returns.
Make sure you have a follow-up appointment scheduled with your heart care provider (cardiologist).
Your provider may refer you to a cardiac rehabilitation program. This will help you learn how to slowly increase your exercise. You will also learn how to take care of your angina and care for yourself after a heart attack.
When to Call the Doctor
Contact your provider if:
- There is bleeding at the catheter insertion site that does not stop when you apply pressure.
- There is swelling at the catheter site.
- Your leg or arm below where the catheter was inserted changes color, becomes cool to touch, or is numb.
- The small incision for your catheter becomes red or painful, or yellow or green discharge is draining from it.
- You have chest pain or shortness of breath that does not go away with rest.
- Your pulse feels irregular -- very slow (fewer than 60 beats), or very fast (over 100 to 120 beats) a minute.
- You have dizziness, fainting, or you are very tired.
- You are coughing up blood or yellow or green mucus.
- You have problems taking any of your heart medicines.
- You have chills or a fever over 101°F (38.3°C).
Related Information
Angioplasty and stent placement - carotid arteryHeart attack
Unstable angina
High blood cholesterol levels
High blood pressure in adults - hypertension
Angina
Heart bypass surgery
Heart bypass surgery - minimally invasive
Tips on how to quit smoking
Stent
Angina - discharge
Heart attack – discharge
Angioplasty and stent - heart - discharge
Aspirin and heart disease
Being active when you have heart disease
Butter, margarine, and cooking oils
Cardiac catheterization - discharge
Antiplatelet medicines - P2Y12 inhibitors
ACE inhibitors
Angina - when you have chest pain
Being active after your heart attack
Cholesterol and lifestyle
Controlling your high blood pressure
Dietary fats explained
Fast food tips
Heart disease - risk factors
How to read food labels
Mediterranean diet
Angina - what to ask your doctor
Heart attack - what to ask your provider
References
Bohula EA, Morrow DA. ST-elevation myocardial infarction: management. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 38.
Dangas GD, Mehran R. Coronary angiography and intravascular imaging. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 21.
Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 39.
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454. PMID: 34709928 pubmed.ncbi.nlm.nih.gov/34709928/.
Kumbhani DJ, Bhatt DL. Percutaneous coronary intervention. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 41.
Virani SS, Newby K, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2023 Aug 29;148(9):e9-e119. PMID: 37471501 pubmed.ncbi.nlm.nih.gov/37471501/.
BACK TO TOPReview Date: 8/5/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
