Ileostomy - caring for your stoma
Standard ileostomy - stoma care; Brooke ileostomy - stoma care; Continent ileostomy - stoma care; Abdominal pouch - stoma care; End ileostomy - stoma care; Ostomy - stoma care; Crohn's disease - stoma care; Inflammatory bowel disease - stoma care; Regional enteritis - stoma care; IBD - stoma care
Images
Description
You had an injury or disease of your digestive system and needed an operation called an ileostomy. The operation changes the way your body gets rid of waste (stool, feces, or poop).
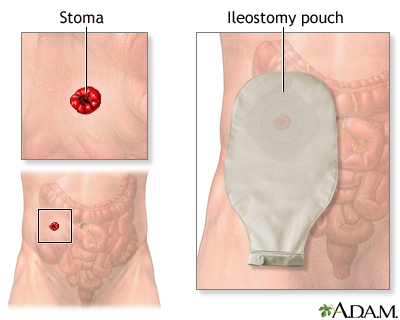
Now you have an opening called a stoma in your belly. Waste will pass through the stoma into a pouch that collects it. You will need to take care of your stoma and empty the pouch several times a day.
About Your Stoma
Things to know about your stoma include:
- The surface of your stoma is the lining of your intestine.
- It will be pink or red, moist, and a little shiny.
- Stomas are most often round or oval.
- A stoma is very delicate.
- Most stomas stick out a little over the skin, but some are flat.
- You may see a little mucus. Your stoma may bleed a little when you clean it.
- The skin around your stoma should be dry.
The feces that come out of the stoma can be very irritating to the skin. So it is important to take special care of the stoma to avoid damage to the skin.
Stoma Care
After surgery, the stoma will be swollen. It will shrink over the next several weeks.
The skin around your stoma should look like it did before surgery. The best way to protect your skin is by:
- Using a bag or pouch with the correct size opening, so waste does not leak
- Taking good care of the skin around your stoma
Stoma appliances are either 2-piece or 1-piece sets. A 2-piece set consists of a baseplate (or wafer) and pouch. A baseplate is the part that sticks to the skin and protects it against irritation from feces. The second piece is the pouch into which feces empty. The pouch attaches to the baseplate, similar to a Tupperware cover. In a 1-piece set, the baseplate and appliance is all one piece. The baseplate usually needs to be changed only once or twice a week.
To care for your skin:
- Wash your skin with warm water and pat dry it well before you attach the pouch.
- Avoid skin care products that contain alcohol. These can make your skin too dry.
- Do not use products that contain oil on the skin around your stoma. Doing so can make it hard to attach the pouch to your skin.
- Use special skin care products to make skin problems less likely.
If you have hair on the skin around your stoma, your pouch may not stick. Removing the hair may help.
- Ask your ostomy nurse about the best way to shave the area.
- If you use a safety razor and soap or shaving cream, be sure to rinse your skin well after you shave the area.
- You can also use trimming scissors, electric shaver, or have laser treatment to remove the hair.
- Do not use a straight edge.
- Be careful to protect your stoma if you remove the hair around it.
Carefully look at your stoma and the skin around it every time you change your pouch or barrier. If the skin around your stoma is red or wet, your pouch may not be sealed well on your stoma.
Sometimes the adhesive, skin barrier, paste, tape, or pouch may damage the skin. This may happen when you first start using a stoma, or it may happen after you have been using it for months, or even years.
If this happens:
- Ask your health care provider about medicine to treat your skin.
- Call your provider if it is does not get better when you treat it.
If your stoma is leaking, your skin will get sore.
Be sure to treat any skin redness or skin changes right away, when the problem is still small. Do not allow the sore area to become larger or more irritated before asking your provider or ostomy nurse about it.
If your stoma becomes longer than usual (sticks out from the skin more), try a cold compress, like ice wrapped in a towel, to make it go in.
You should never stick anything into your stoma, unless your doctor tells you to.
When to Call the Doctor
Contact your provider if:
- Your stoma is swollen and is more than a 1/2 inch (1 cm) larger than normal.
- Your stoma is pulling in, below the skin level.
- Your stoma is bleeding more than normal.
- Your stoma has turned purple, black, or white.
- Your stoma is leaking often or draining fluid.
- Your stoma does not seem to fit as well as it did before.
- You have to change the appliance once every day or two.
- You have a discharge from the stoma that smells bad.
- You have any signs of being dehydrated (there is not enough water in your body). Some signs are dry mouth, urinating less often, and feeling lightheaded or weak.
- You have diarrhea that is not going away.
Contact your provider if the skin around your stoma:
- Pulls back
- Is red or raw
- Has a rash
- Is dry
- Hurts or burns
- Swells or pushes out
- Bleeds
- Itches
- Has white, gray, brown, or dark red bumps on it
- Has bumps around a hair follicle that are filled with pus
- Has sores with uneven edges
Also contact your provider if you:
- Have less waste than usual in your pouch
- Have a fever
- Experience any abdominal or stoma-area pain
- Have any questions or concerns about your stoma or skin
Related Information
Intestinal obstruction repairLarge bowel resection
Small bowel resection
Ileostomy
Total abdominal colectomy
Total proctocolectomy and ileal-anal pouch
Total proctocolectomy with ileostomy
Crohn disease
Ulcerative colitis
Colorectal cancer
Ileostomy and your child
Ileostomy and your diet
Types of ileostomy
Ileostomy - discharge
Living with your ileostomy
Large bowel resection - discharge
Small bowel resection - discharge
Total colectomy or proctocolectomy - discharge
Bland diet
Ileostomy - changing your pouch
Crohn disease - discharge
Ulcerative colitis - discharge
Ileostomy - what to ask your doctor
References
Beck DE. Ostomy construction and management: personalizing the stoma for the patient. In: Yeo CJ, ed. Shackelford's Surgery of the Alimentary Tract. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 178.
Lyon CC. Stoma care. In: Lebwohl MG, Heymann WR, Coulson IH, Murrell DF, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 6th ed. Philadelphia, PA: Elsevier; 2022:chap 232.
Raza A, Araghizadeh F. Ileostomy, colostomy, pouches, and anastomoses. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 117.
BACK TO TOPReview Date: 6/11/2024
Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
