Disk replacement - lumbar spine
Lumbar disk arthroplasty; Thoracic disk arthroplasty; Artificial disk replacement; Total disk replacement; TDR; Disc arthroplasty; Disc replacement; Artificial disc
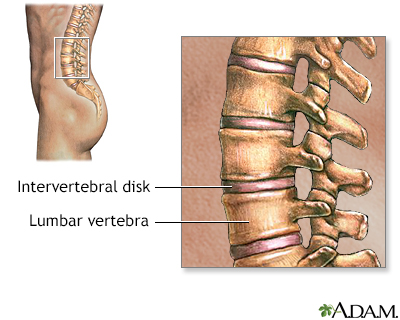
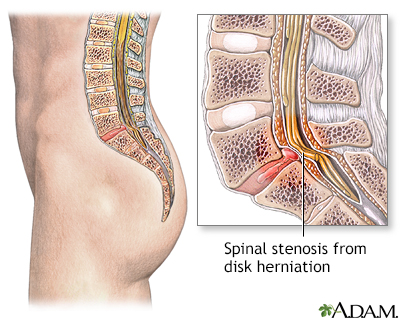
Lumbar spine disk replacement is surgery of the lower back (lumbar) area. It is done to treat spinal stenosis or disk problems and allow normal movement of the backbone.
Spinal stenosis is present when:
- The space for the spinal column is narrowed.
- The openings for the nerve roots leaving the spinal column become narrow, placing pressure on the nerve.
Images
I Would Like to Learn About:
Description
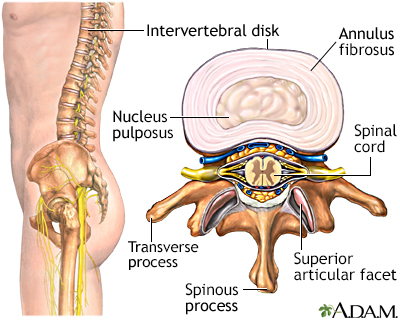
During total disk replacement (TDR), the inner portion of a damaged spinal disk is replaced with an artificial disk to restore normal movement of the backbone.
Most often, surgery is done for only one disk, but at times, two levels next to each other may be replaced.
The surgery is done under general anesthesia. You will be asleep and not feel any pain.
During surgery:
- You will lie on your back on the operating table.
- Your arms are padded at the elbow area and folded in front of your chest.
- Your surgeon makes an incision (cut) on your abdomen. Doing the operation through the abdomen allows the surgeon to access the spine without disturbing the spinal nerves.
- The gut organs and blood vessels are moved to the side to get access to the backbone.
- Your surgeon removes the damaged portion of the disk and puts the new artificial disk in its place.
- All the organs are put back into place.
- The incision is closed with stitches.
The surgery takes about 2 hours to complete.
Why the Procedure Is Performed
Cushion-like disks help the spine stay mobile. Nerves in the lower spine area get compressed due to:
- Narrowing of the disk due to old injuries
- Bulging of the disk (protrusion)
- Arthritis that occurs in your spine that pushes on the nerves
Surgery for spinal stenosis may be considered if you have severe symptoms that interfere with your daily life and do not improve with other therapy. Symptoms most often include:
- Pain that may be felt in your thigh, calf or lower back. The pain is often deep and steady.
- Pain when doing certain activities or moving your body a certain way.
- Numbness, tingling, and muscle weakness.
- Difficulty with balance and walking.
- Loss of bladder or bowel control.
Talk to your health care provider about whether surgery is right for you. Most people with lower back pain do not need surgery. Most people are first treated with medicines, physical therapy, and exercise for relief of back pain.
During traditional spinal surgery for spinal stenosis, the surgeon will need to fuse some of the bones in your spine to make your spine more stable. As a result, other parts of your spine below and above the fusion may be more likely to have disk problems in the future.
With disk replacement surgery, no fusion is needed. As a result, the spine above and below the site of surgery still has preserved movement. This movement may help prevent further disk problems.
You may be a candidate for disk replacement surgery if the following are true:
- You are not very overweight.
- Only one or two levels of your spine have this problem and other areas did not.
- You do not have a lot of arthritis in the joints of your spine.
- You have not had spine surgery in the past.
- You do not have severe pressure on the nerves of your spine.
Risks
Risks of anesthesia and surgery in general are:
- Allergic reaction to medicines
- Breathing problems
- Bleeding, blood clots, and infection
Risks for TDR are:
- Increase in back pain
- Difficulty with movement
- Injury to the gut
- Blood clots in legs
- Abnormal bone formation in the muscles and tendons surrounding the spinal cord
- Sexual dysfunction (more common in men)
- Damage to the ureter and bladder
- Infection at the surgical site
- Breakage of the artificial disk
- Artificial disk may move out of place
- Loosening of the implant
- Paralysis
Before the Procedure
Your provider will order an imaging test such as an MRI, CT scan, or x-ray to check if you need surgery.
Your provider will want to know if you:
- Are pregnant
- Are taking any medicines, supplements, or herbs
- Are diabetic, hypertensive, or have any other medical condition
- Are a smoker
Tell your provider what medicines you are taking. This includes medicines, supplements, or herbs you bought without a prescription.
During the days before the surgery:
- Prepare your home for when you leave the hospital.
- If you are a smoker, you need to stop. People who have TDR and continue to smoke may not heal as well. Ask your provider for help quitting.
- One week before surgery, your provider may ask you to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn).
- If you have diabetes, heart disease, or other medical problems, your surgeon will ask you to see the provider who treats these conditions to determine if surgery is safe for you.
- Talk with your provider if you have been drinking a lot of alcohol.
- Ask your surgeon which medicines you should still take on the day of the surgery.
- Let your surgeon know right away if you get a cold, flu, fever, herpes breakout, or other illnesses you may have.
- You may want to visit a physical therapist to learn exercises to do before surgery.
On the day of the surgery:
- Follow instructions on not drinking or eating anything before the procedure. This may be 6 to 12 hours before surgery.
- Take the medicines your provider told you to take with a small sip of water.
- Your surgeon will tell you when to arrive at the hospital. Be sure to arrive on time.
After the Procedure
You will stay in the hospital 1 to 2 days after surgery. Your surgeon will encourage you to stand and start walking as soon as the anesthesia wears off. You may have to wear a corset brace for support and faster healing. In the beginning, you'll be given clear liquids. You'll later progress to a liquid and semi-solid diet.
Your surgeon will ask you not to:
- Do any activity that stretches your spine too much
- Take part in activities that involve jarring, bending, and twisting such as driving and lifting heavy objects for at least 3 months after surgery
Follow instructions on how to take care of your back at home.
You can likely return to normal activities 3 months after the surgery.
Outlook (Prognosis)
The risk of complications are low after lumbar disk replacement. The surgery usually improves movement of the backbone better than other (spine surgeries). It is a safe procedure and pain relief occurs soon after surgery. The risk of spinal muscle (paravertebral muscle) injury is less than with other types of spine surgeries.
References
Derman PB, Zigler Je, Guyer RD, Blumenthal S, Lieberman IH. Lumbar disk arthroplasy. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 356.
Duffy MF, Zigler JE. Lumbar total disk arthroplasty. In: Baron EM, Vaccaro AR, eds. Operative Techniques: Spine Surgery.3rd ed. Philadelphia, PA: Elsevier; 2018:chap 42.
Gardocki RJ, Park AL. Degenerative disorders of the thoracic and lumbar spine. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 39.
Johnson R, Guyer RD. Lumbar disc degeneration: Anterior lumbar interbody fusion, degeneration, and disc replacement. In: Garfin SR, Eismont FJ, Bell GR, Fischgrund JS, Bono CM, eds. Rothman-Simeone and Herkowitz's The Spine. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 49.
Zigler J, Gornet MF, Ferko N, Cameron C, Schranck FW, Patel L. Comparison of lumbar total disc replacement with surgical spinal fusion for the treatment of single-level degenerative disc disease: a meta-analysis of 5-year outcomes from randomized controlled trials. Global Spine J. 2018;8(4):413-423. PMID: 29977727 pubmed.ncbi.nlm.nih.gov/29977727/.
BACK TO TOPReview Date: 9/20/2022
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
