Esophagectomy - minimally invasive
Minimally invasive esophagectomy; Robotic esophagectomy; Removal of the esophagus - minimally invasive; Achalasia - esophagectomy; Barrett esophagus - esophagectomy; Esophageal cancer - esophagectomy - laparoscopic; Cancer of the esophagus - esophagectomy - laparoscopic
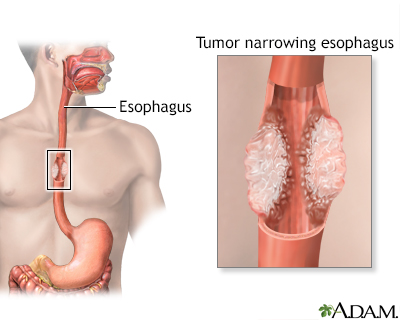
Minimally invasive esophagectomy is surgery to remove part or all of the esophagus. This is the tube that moves food from your throat to your stomach. After it is removed, the esophagus is rebuilt from part of your stomach or part of your large intestine.
Most of the time, esophagectomy is done to treat cancer of the esophagus. The surgery may also be done to treat the esophagus if it is no longer working to move food into the stomach.
Images
Description
During minimally invasive esophagectomy, small surgical cuts (incisions) are made in your upper belly, chest, or neck. A viewing scope (laparoscope) and surgical tools are inserted through the incisions to perform the surgery. (Removal of the esophagus can also be done using the open method. Surgery is done through larger incisions.)
Laparoscopic surgery is generally done in the following way:
- You'll receive general anesthesia at the time of your surgery. This will keep you asleep and pain-free.
- The surgeon makes 3 to 4 small cuts in your upper belly, chest, or lower neck. These cuts are about 1-inch (2.5 cm) long.
- The laparoscope is inserted through one of the cuts into your upper belly. The scope has a light and camera on the end. Video from the camera appears on a monitor in the operating room. This allows the surgeon to view the area being operated on. Other surgical tools are inserted through the other cuts.
- The surgeon frees the esophagus from nearby tissues. Depending on how much of your esophagus is diseased, part or most of it is removed.
- If part of your esophagus is removed, the remaining ends are joined together using staples or stitches. If most of your esophagus is removed, the surgeon reshapes your stomach into a tube to make a new esophagus. It is joined to the remaining part of the esophagus.
- During surgery, lymph nodes in your chest and belly are likely removed to determine if cancer has spread to them.
- A feeding tube is placed in your small intestine so that you can be fed while you are recovering from surgery.
Some medical centers do this operation using robotic surgery. In this type of surgery, a small scope and other instruments are inserted through the small cuts in the skin. The surgeon controls the scope and instruments while sitting at a computer station and viewing a monitor.
Surgery usually takes 3 to 6 hours.
Why the Procedure Is Performed
The most common reason for removing part, or all, of your esophagus is to treat cancer of the esophagus. You may also have radiation therapy or chemotherapy before or after surgery.
Surgery to remove the lower esophagus may also be done to treat:
- A condition in which the ring of muscle in the esophagus does not work well (achalasia)
- Severe damage of the lining of the esophagus that can lead to cancer (Barrett esophagus)
- Severe trauma
Risks
This is major surgery and has many risks. Some of them are serious. Be sure to discuss these risks with your surgeon.
Risks for this surgery, or for problems after surgery, may be higher than normal if you:
- Are unable to walk even for short distances (this increases the risk for blood clots, lung problems, and pressure sores)
- Are older than 60 years
- Are a heavy smoker
- Are obese
- Have lost a lot of weight from your cancer
- Are on steroid medicines
- Have had a severe infection from the damaged esophagus/stomach
- Had cancer drugs (chemotherapy) before the surgery
Risks for anesthesia and surgery in general are:
- Allergic reactions to medicines
- Breathing problems
- Bleeding, blood clots, or infection
Risks for this surgery are:
- Acid reflux
- Injury to the stomach, intestines, lungs, or other organs during surgery
- Leakage of the contents of your esophagus or stomach where the surgeon joined them together
- Narrowing of the connection between your stomach and esophagus
- Pneumonia
- Difficulty swallowing or speaking
- Bowel obstruction
Before the Procedure
You will have many medical visits and tests before you have surgery. Some of these are:
- A complete physical examination.
- Visits with your health care provider to make sure other medical problems you may have, such as diabetes, high blood pressure, and heart or lung problems, are under control.
- Nutritional counseling.
- A visit or class to learn what happens during surgery, what you should expect afterward, and what risks or problems may occur afterward.
- If you have recently lost weight, your doctor may put you on oral or IV nutrition for several weeks before surgery.
- CT scan to look at the esophagus.
- PET scan to identify the cancer and if it has spread.
- Endoscopy to diagnose and identify how far the cancer has gone.
If you are a smoker, you should stop several weeks before surgery. Ask your provider for help.
Tell your provider:
- If you are or might be pregnant.
- What medicines, vitamins, and other supplements you are taking, even ones you bought without a prescription.
- If you have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
During the week before surgery:
- You may be asked to stop taking blood thinner drugs. Some of these are aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and clopidogrel (Plavix).
- Ask your surgeon which medicines you should still take on the day of surgery.
- Prepare your home for after surgery.
On the day of surgery:
- Follow instructions on when to stop eating and drinking before surgery.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
Most people stay in the hospital for 7 to 14 days after an esophagectomy. How long you stay will depend on what type of surgery you had. You may spend 1 to 3 days in the intensive care unit (ICU) right after surgery.
During your hospital stay, you will:
- Be asked to sit on the side of your bed and walk on the same day or day after surgery.
- Not be able to eat for at least the first 2 to 7 days after surgery. After that, you may be able to start with liquids. You will be fed through a feeding tube that was placed into your intestine during surgery.
- Have a tube coming out of the side of your chest to drain fluids that build up.
- Wear special stockings on your feet and legs to prevent blood clots.
- Receive shots to prevent blood clots.
- Receive pain medicine through an IV or take pills. You may receive your pain medicine through a special pump. With this pump, you press a button to deliver pain medicine when you need it. This allows you to control the amount of pain medicine you get.
- Do breathing exercises.
After you go home, follow instructions on how to take care of yourself as you heal. You'll be given information on diet and eating. Be sure to follow those instructions as well.
Outlook (Prognosis)
Many people recover well from this surgery and can have a fairly normal diet. After they recover, they will likely need to eat smaller portions and eat more often.
If you had the surgery for cancer, talk with your provider about the next steps to treat the cancer.
Related Information
Esophageal cancerEsophagectomy - open
Gastrostomy feeding tube - bolus
Clear liquid diet
Esophagectomy - discharge
Diet and eating after esophagectomy
References
National Cancer Institute website. Esophageal cancer treatment (PDQ) - health professional version. www.cancer.gov/types/esophageal/hp/esophageal-treatment-pdq. Updated October 14, 2022. Accessed February 28, 2023.
Rajaram R, Spicer JD, Dhupar R, Kim JY, Sepesi B, Hofstetter WL. Esophagus. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 42.
Wilder FG, Yang SC. Management of esophageal cancer. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:54-65.
BACK TO TOPReview Date: 1/23/2023
Reviewed By: Mary C. Mancini, MD, PhD, Cardiothoracic Surgeon, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
