Coronary heart disease
Heart disease, Coronary heart disease, Coronary artery disease; Arteriosclerotic heart disease; CHD; CAD
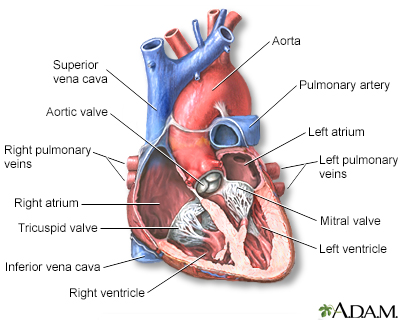
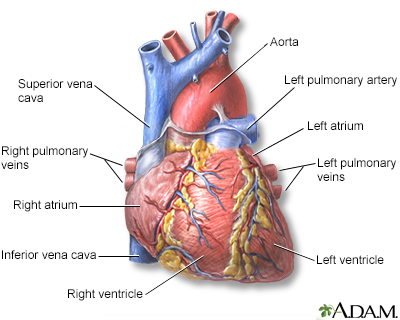
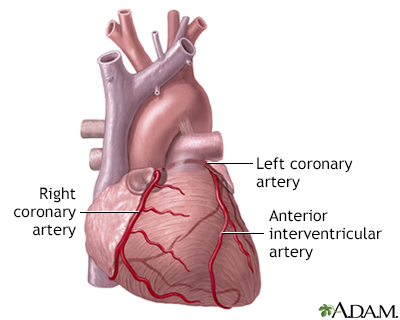
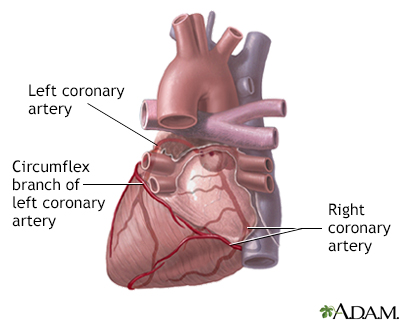
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called coronary artery disease.
Images
I Would Like to Learn About:
Causes
CHD is the leading cause of death in the United States for men and women.
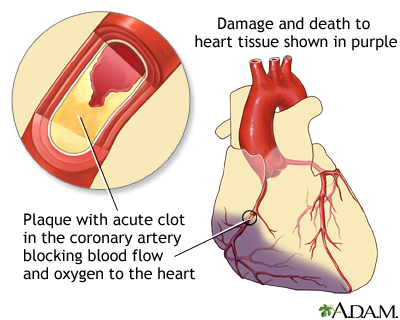
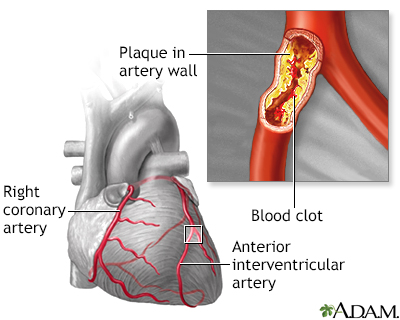
CHD is caused by the buildup of plaque in the arteries to your heart. This may also be called hardening of the arteries or atherosclerosis.
- Fatty material and other substances form a plaque buildup on the walls of your coronary arteries. The coronary arteries bring blood and oxygen to your heart.
- This buildup causes the arteries to get narrow.
- As a result, blood flow to the heart can slow down or stop.
A risk factor for heart disease is something that increases your chance of getting it. You cannot change some risk factors for heart disease, but you can change others.
Symptoms
In some cases, symptoms may be very noticeable. But, you can have the disease and not have any symptoms. This is more often true in the early stages of CHD.
Chest pain or discomfort (angina) is the most common symptom. You feel this pain when the heart is not getting enough blood or oxygen. The pain may feel different from person to person.
- It may feel heavy or like someone is squeezing your heart. You may feel it under your breast bone (sternum). You may also feel it in your neck, arms, stomach, or upper back.
- The pain most often occurs with activity or emotion. It goes away with rest or a medicine called nitroglycerin.
- Other symptoms can include shortness of breath and fatigue with activity (exertion), or even feeling lightheaded or passing out with exertion.
Some people have symptoms other than chest pain, such as:
- Fatigue
- Shortness of breath
- General weakness
Exams and Tests
Your health care provider will examine you. You will often need one or more tests before getting a diagnosis.
Tests to evaluate for CHD may include:
- Coronary angiography -- an invasive test that evaluates the heart arteries under x-ray.
- Echocardiogram stress test.
- Electrocardiogram (ECG).
- Electron-beam computed tomography (EBCT) to look for calcium in the lining of the arteries. The more calcium, the higher your chance for CHD.
- Exercise stress test.
- Heart CT scan.
- Nuclear stress test.
Treatment
You may be asked to take one or more medicines to treat blood pressure, diabetes, or high cholesterol levels. Follow your provider's directions closely to help prevent CHD from getting worse.
Goals for treating these conditions in people who have CHD:
- The most commonly used blood pressure target for people with heart disease is less than 130/80, but your provider may recommend a different blood pressure target.
- If you have diabetes, your HbA1c (glycohemoglobin A1c) blood levels will be monitored and brought down to the level your provider recommends.
- Your LDL cholesterol level will be lowered with statin or other medicines.
Treatment depends on your symptoms and how severe the disease is. You should know about:
- Other medicines used to treat angina.
- What to do when you have chest pain.
- Being active when you have heart disease.
- Eating a heart-healthy diet.
Never stop taking your medicines without first talking to your provider. Stopping heart medicines suddenly can make your angina worse or cause a heart attack.
You may be referred to a cardiac rehabilitation program to help improve your heart's fitness.
Procedures and surgeries used to treat CHD include:
- Angioplasty and stent placement, called percutaneous coronary interventions (PCIs)
- Coronary artery bypass surgery
- Minimally invasive heart surgery
Outlook (Prognosis)
Everyone recovers differently. Some people can stay healthy by changing their diet, stopping smoking, and taking their medicines as prescribed. Others may need medical procedures such as angioplasty or surgery.
In general, early detection of CHD generally leads to a better outcome.
When to Contact a Medical Professional
If you have any risk factors for CHD, talk to your provider about prevention and possible treatment steps.
Call your provider, call the local emergency number (such as 911), or go to the emergency room right away if you have:
- Angina or chest pain
- Shortness of breath
- Symptoms of a heart attack
- Sudden loss of consciousness
Prevention
Take these steps to help prevent heart disease.
- If you smoke or use tobacco, stop. There are many resources available to help you stop smoking or using tobacco.
- Learn how to eat a heart-healthy diet by making simple substitutions. For example, choose heart-healthy fats over butter and other saturated fats.
- Get regular exercise, ideally at least 30 minutes five days per week. If you have heart disease, talk with your provider about starting an exercise routine.
- Maintain a healthy body weight.
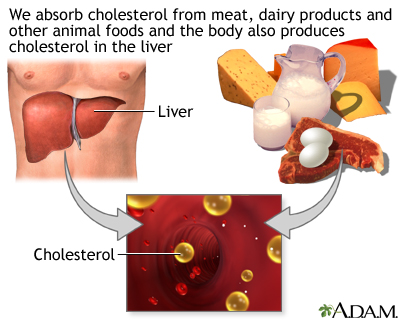
- Lower high cholesterol with lifestyle changes, and if needed, statin or other medicines.
- Lower high blood pressure using diet and medicines.
- Talk with your provider about aspirin therapy.
- If you have diabetes, keep it well-managed to help prevent heart attack and stroke.
Even if you already have heart disease, taking these steps will help protect your heart and prevent further damage.
Related Information
AtherosclerosisStable angina
Heart attack
Heart disease and women
Unstable angina
Magnetic resonance angiography
Ventricular assist device
Cardiac intravascular ultrasound
Metabolic syndrome
Obesity
Gastric bypass surgery
Laparoscopic gastric banding
Gastric bypass surgery - discharge
Laparoscopic gastric banding - discharge
After weight-loss surgery - what to ask your doctor
Before weight-loss surgery - what to ask your doctor
Cholesterol - drug treatment
Aspirin and heart disease
Heart pacemaker - discharge
Antiplatelet medicines - P2Y12 inhibitors
Controlling your high blood pressure
Heart bypass surgery - discharge
Heart bypass surgery - minimally invasive - discharge
Dietary fats explained
Fast food tips
Heart disease - risk factors
How to read food labels
Implantable cardioverter defibrillator - discharge
Low-salt diet
Mediterranean diet
Heart failure - fluids and diuretics
Heart failure - home monitoring
Heart failure - discharge
References
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. [published correction appears in Circulation. 2019;140(11):e649-e650] [published correction appears in Circulation. 2020;141(4):e60] [published correction appears in Circulation. 2020;141(16):e774]. Circulation. 2019 2019;140(11):e596-e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Boden WE. Angina pectoris and stable ischemic heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 56.
Marks AR. Cardiac and circulatory function. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 41.
Morrow DA, de Lemos J. Stable ischemic heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 40.
Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology joint committee on clinical practice guidelines. Circulation. 2023;148:e9–e119.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;72(3):e33. PMID: 29133354 pubmed.ncbi.nlm.nih.gov/29133354/.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: Larry A. Weinrauch MD, Assistant Professor of Medicine, Harvard Medical School, Cardiovascular Disease and Clinical Outcomes Research, Watertown, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
