Hypospadias repair
Urethroplasty; Meatoplasty; Glanuloplasty
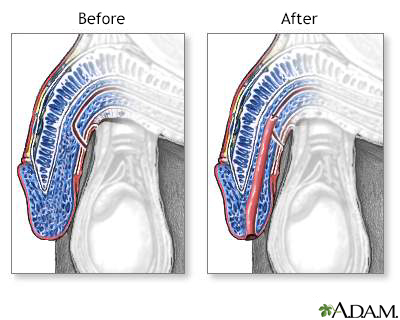
Hypospadias repair is surgery to correct a defect in the opening of the penis that is present at birth. The urethra (the tube that carries urine from the bladder to outside the body) does not end at the tip of the penis. Instead, it ends on the underside of the penis. In more severe cases, the urethra opens at the middle or bottom of the penis, or in or behind the scrotum.
Images
Presentation

Description
Hypospadias repair is done most often when boys are between 6 months and 2 years old. The surgery is done as an outpatient. The child rarely has to spend a night in the hospital. Boys who are born with hypospadias should not be circumcised at birth. The extra tissue of the foreskin may be needed to repair the hypospadias during surgery.
Before surgery, your child will receive general anesthesia. This will make him sleep and make him unable to feel pain during surgery. Mild defects may be repaired in one procedure. Severe defects may need two or more procedures.
The surgeon will use a small piece of foreskin or tissue from another site to create a tube that increases the length of the urethra. Extending the length of the urethra will allow it to open at the tip of the penis.
During surgery, the surgeon may place a catheter (tube) in the urethra to make it hold its new shape. The catheter may be sewn or fastened to the head of the penis to keep it in place. It will be removed 1 to 2 weeks after surgery.
Most of the stitches used during surgery will dissolve on their own and will not have to be removed later.
Why the Procedure Is Performed
Hypospadias is one of the most common birth defects in boys. This surgery is performed on most boys who are born with the problem.
If the repair is not done, problems may occur later on such as:
- Difficulty controlling and directing urine stream
- A curve in the penis during erection
- Decreased fertility
- Embarrassment about appearance of penis
Surgery is not needed if the condition does not affect normal urination while standing, sexual function, or the deposit of semen.
Risks
Risks for this procedure include:
- A hole that leaks urine (fistula)
- Large blood clot (hematoma)
- Scarring or narrowing of the repaired urethra
Before the Procedure
Your child's health care provider may ask for a complete medical history and do a physical exam before the procedure.
Always tell your child's provider:
- What medicines your child is taking
- Medicines, herbs, and vitamins your child is taking that you bought without a prescription
- Any allergies your child has to medicine, latex, tape, or skin cleaner
Ask your child's provider which medicines your child should still take on the day of surgery.
On the day of the surgery:
- Your child will most often be asked not to drink or eat anything after midnight the night before surgery or 6 to 8 hours prior to surgery.
- Give your child any medicines your provider told you to give your child with a small sip of water.
- You will be told when to arrive for the surgery.
- The provider will make sure your child is healthy enough for surgery. If your child is ill, the surgery may be delayed.
After the Procedure
Right after surgery, your child's penis may be taped to his belly so that it does not move.
Often, a bulky dressing or plastic cup is placed over the penis to protect the surgical area. A urinary catheter (a tube used to drain urine from the bladder) will be put through the dressing so urine can flow into the diaper.
Your child will be encouraged to drink fluids so that he will urinate. Urinating will keep pressure from building up in the urethra.
Your child may be given medicine to relieve pain. Most of the time, the child can leave the hospital the same day as the surgery. If you live a long way from the hospital, you may want to stay in a hotel near the hospital for the first night after the surgery.
Your child's provider will explain how to take care of your child at home after leaving the hospital.
Outlook (Prognosis)
This surgery lasts a lifetime. Most children do well after this surgery. The penis will look almost or completely normal and function well.
If your child has a complicated hypospadias, he may need more operations to improve the penis appearance or to repair a hole or narrowing in the urethra.
Follow-up visits with a urologist may be needed after the surgery has healed. Boys will sometimes need to visit the urologist when they reach puberty.
Related Information
HypospadiasPenis
Circumcision
Surgical wound care - open
Kegel exercises - self-care
Hypospadias repair - discharge
References
Carrasco A, Murphy JP. Hypospadias. In: Holcomb GW, Murphy JP, St. Peter SD, eds. Holcomb and Ashcraft's Pediatric Surgery. 7th ed. Philadelphia, PA: Elsevier; 2020:chap 59.
Elder JS. Anomalies of the penis and urethra. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 559.
Long CJ, Zaontz MR, Canning DA. Hypospadias. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 45.
Thomas JC, Brock JW. Repair of proximal hypospadias. In: Smith JA Jr, Howards SS, Preminger GM, Dmochowski RR, eds. Hinman's Atlas of Urologic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 130.
BACK TO TOPReview Date: 7/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
