Spinal fusion
Vertebral interbody fusion; Posterior spinal fusion; Arthrodesis; Anterior spinal fusion; Spine surgery - spinal fusion; Low back pain - fusion; Herniated disk - fusion; Spinal stenosis - fusion; Laminectomy - fusion; Cervical spinal fusion; Lumbar spinal fusion
Spinal fusion is surgery to permanently join together two or more bones in the spine so there is no movement between them. These bones are called vertebrae.
Images
Presentation

Description
You'll be given general anesthesia, which puts you into a deep sleep so you do not feel pain during surgery.
The surgeon will make a surgical cut (incision) to view the spine. Other surgery, such as a diskectomy, laminectomy, or a foraminotomy, is almost always done first. Spinal fusion may be done:
- On the part of your back or neck over the spine. You may be lying face down. Muscles and tissue will be separated to expose the spine.
- On your side, if you are having surgery on your lower back. The surgeon will use tools called retractors to gently separate, hold the soft tissues such as your bowels and blood vessels apart, and have room to work.
- With a cut on the front of the neck, toward the side.
The surgeon will use a graft (such as bone) to hold (or fuse) the bones together permanently. There are several ways of fusing vertebrae together:
- Strips of bone graft material may be placed over the back part of the spine.
- Bone graft material may be placed between the vertebrae.
- Special cages may be placed between the vertebrae. These implantable cages are packed with bone graft material.
The surgeon may get the bone graft from:
- Another part of your body (usually around your pelvic bone). This is called an autograft. Your surgeon will make a small cut over your pelvic bone and remove some bone from the back of the rim of the pelvis.
- A bone bank. This is called an allograft which is bone taken from other people that has been cleaned and preserved.
- An artificial bone substitute and growth factors.
The vertebrae may also be fixed together with rods, screws, plates, or cages. They are used to keep the vertebrae from moving until the bone grafts are fully healed.
Surgery can take 3 to 4 hours.
Why the Procedure Is Performed
Spinal fusion is most often done along with other surgical procedures of the spine. It may be done:
- With other surgical procedures for spinal stenosis, such as foraminotomy or laminectomy
- After diskectomy in the neck
Spinal fusion may be done if you have:
- Injury or fractures to the bones in the spine
- Weak or unstable spine caused by infections or tumors
- Spondylolisthesis, a condition in which one vertebrae slips forward on top of another
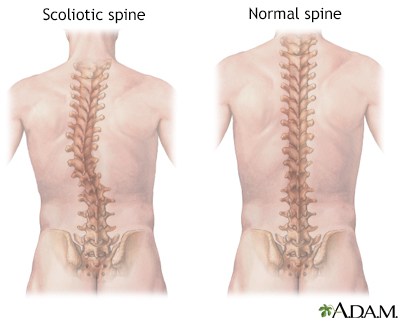
- Abnormal curvatures, such as those from scoliosis or kyphosis
- Arthritis in the spine, such as spinal stenosis
You and your surgeon can decide when you need to have surgery.
Risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines, breathing problems
- Bleeding, blood clots, infection
Risks for this surgery include:
- Infection in the wound or vertebral bones
- Damage to a spinal nerve, causing weakness, pain, loss of sensation, problems with your bowels or bladder
- The vertebrae above and below the fusion are more likely to wear away, leading to more problems later
- Leakage of spinal fluid that may require more surgery
- Headaches
Before the Procedure
Tell your surgeon what medicines you are taking. These include medicines, herbs, and supplements you bought without a prescription.
During the days before the surgery:
- Prepare your home for when you leave the hospital.
- If you are a smoker, you need to stop. People who have spinal fusion and continue to smoke may not heal as well. Ask your surgeon or health care provider for help.
- Two weeks before surgery, your surgeon may ask you to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and other medicines like these.
- If you have diabetes, heart disease, or other medical problems, your surgeon will ask you to see your regular provider.
- Talk with your surgeon or provider if you have been drinking a lot of alcohol.
- Ask your surgeon which medicines you should still take on the day of the surgery.
- Let your surgeon know about any cold, flu, fever, herpes breakout, or other illnesses you may have.
On the day of the surgery:
- Follow instructions about not drinking or eating anything before the procedure.
- Take the medicines you were told to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You may stay in the hospital for up to 3 to 4 days after surgery.
You will receive pain medicines in the hospital. You may take pain medicine by mouth or have a shot or an intravenous line (IV). You may have a pump that allows you to control how much pain medicine you get.
You will be taught how to move properly and how to sit, stand, and walk. You will be told to use a "log-rolling" technique when getting out of bed. This means that you move your entire body at once, without twisting your spine.
You may not be able to eat regular food for 2 to 3 days. You will be given nutrients through an IV and will also eat softer food. When you leave the hospital, you may need to wear a back brace or cast.
Your surgeon will tell you how to take care of yourself at home after spine surgery. Follow instructions on how to take care of your back at home.
Outlook (Prognosis)
Surgery does not always improve pain, and in some cases, can make it worse. However, in some people, surgery can be effective for severe pain that does not get better with other treatments.
If you had chronic back pain before surgery, you will likely still have some pain afterward. Spinal fusion is unlikely to take away all your pain and other symptoms.
It is hard to predict which people will improve and how much relief surgery will provide, even when using MRI scans or other tests.
Losing weight and getting exercise increase your chances of feeling better.
Future spine problems are possible after spine surgery. After spinal fusion, the area that was fused together can no longer move. Therefore, the spinal column above and below the fusion are more likely to be stressed when the spine moves, and may cause problems later on.
Related Information
ScoliosisKyphosis
Bone graft
Anterior
Herniated disk
Osteoarthritis
Spinal stenosis
Sciatica
Taking care of your back at home
Neck pain
Diskectomy
Laminectomy
Foraminotomy
Low back pain - acute
Low back pain - chronic
Bathroom safety for adults
Surgical wound care - open
Preventing falls
Spine surgery - discharge
Preventing falls - what to ask your doctor
References
Dru AB, Vaziri S, Polifka AJ, Ghogawala Z, Hoh DJ. Indications for spine fusion for axial pain. In: Steinmetz MP, Berven SH, Benzel EC, eds. Benzel's Spine Surgery: Techniques, Complication Avoidance, and Management. 5th ed. Philadelphia, PA: Elsevier; 2022:chap 135.
Gardocki RJ, Park AL. Degenerative disorders of the thoracic and lumbar spine. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 39.
Wang JC, Dailey AT, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014;21(1):48-53. PMID: 24980585 pubmed.ncbi.nlm.nih.gov/24980585/.
BACK TO TOPReview Date: 8/12/2023
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
