Cervical polyps
Vaginal bleeding - polyps
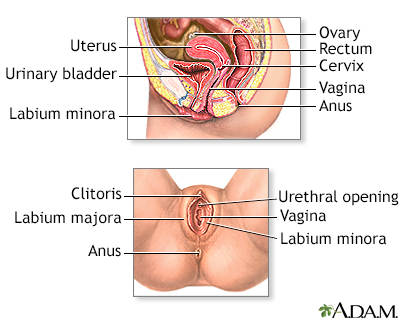
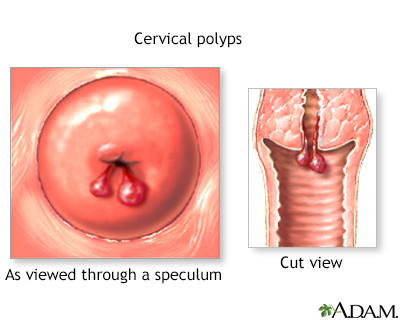
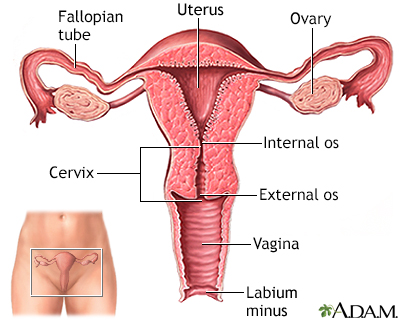
Cervical polyps are fingerlike growths on the lower part of the uterus that connects with the vagina (cervix).
Images
Causes
The exact cause of cervical polyps is not known. They may occur with:
- An abnormal response to increased levels of the female hormone estrogen
- Chronic inflammation
- Clogged blood vessels in the cervix
Cervical polyps are common. They are often found in women over age 40 who have had many children. Polyps are rare in young women who have not started having their period (menstruation).
Symptoms
Polyps do not always cause symptoms. When symptoms are present, they may include:
- Very heavy menstrual periods
- Vaginal bleeding after douching or intercourse
- Abnormal vaginal bleeding after menopause or between periods
- White or yellow mucus (leukorrhea)
Exams and Tests
Your health care provider will perform a pelvic exam. Some smooth, red or purple fingerlike growths will be seen on the cervix.
Most often, the provider will remove the polyp with a gentle tug and send it for testing (biopsy). Most of the time, the biopsy will show cells that are consistent with a benign polyp. Rarely, there may be abnormal, precancerous, or cancer cells in a polyp.
Treatment
The provider can remove polyps during a simple outpatient procedure.
- Smaller polyps may be removed with gentle twisting.
- Electrocautery may be needed to remove larger polyps.
The removed polyp tissue should be sent to a lab for further tests.
Outlook (Prognosis)
Most polyps are not cancerous (benign) and are easy to remove. Polyps do not grow back most of the time. Women who have polyps are at risk of growing more polyps.
Possible Complications
There may be bleeding and slight cramping for a few days after removal of a polyp. Some cervical cancers may first appear as a polyp. Certain uterine polyps may be associated with uterine cancer.
When to Contact a Medical Professional
Contact your provider if you have:
- Abnormal bleeding from the vagina, including bleeding after sex or between periods
- Abnormal discharge from the vagina
- Abnormally heavy periods
- Bleeding or spotting after menopause
Contact your provider to schedule regular gynecological exams. Ask how often you should receive a Pap test.
Prevention
See your provider to treat infections as soon as possible.
Related Information
CervixChronic
References
Choby BA. Cervical polyps. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 123.
Dolan MS, Hill CC, Valea FA. Benign gynecologic lesions: vulva, vagina, cervix, uterus, oviduct, ovary, ultrasound imaging of pelvic structures. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 18.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
