Ventricular septal defect
VSD; Interventricular septal defect; Congenital heart defect - VSD
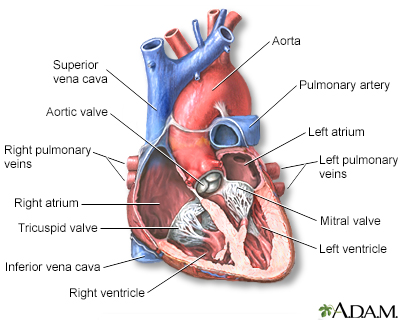
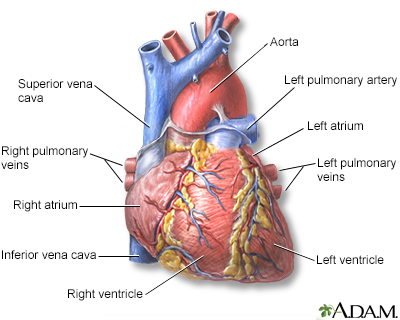
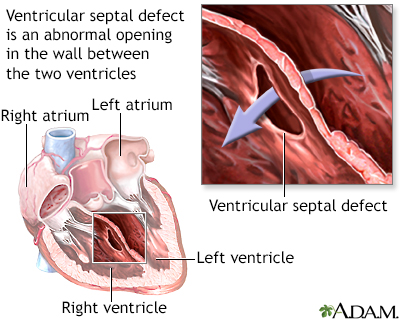
Ventricular septal defect is a hole in the wall that separates the right and left ventricles of the heart. Ventricular septal defect is one of the most common congenital (present from birth) heart defects. It occurs in nearly half of all children with congenital heart disease. It may occur by itself or with other congenital diseases.
Images
Causes
Before a baby is born, the right and left ventricles of the heart are not separate. As the fetus grows, a septum (wall) forms to separate these 2 ventricles. If the wall does not completely form, a hole remains. This hole is known as a ventricular septal defect, or a VSD. The hole can occur in different locations along the septal wall. There can be a single hole or multiple holes.
Ventricular septal defect is a common congenital heart defect. The baby may have no symptoms and the hole can close over time as the wall continues to grow after birth. If the hole is large, too much blood will be pumped to the lungs. This can lead to heart failure. If the hole is small, it may not be detected for years and only discovered in adulthood.
The cause of VSD is not yet known. This defect often occurs along with other congenital heart defects.
In adults, VSDs can be rare, but serious, complication of heart attacks. These holes do not result from a birth defect.
Symptoms
People with VSDs may not have symptoms. However, if the hole is large, the baby often has symptoms related to heart failure.
The most common symptoms include:
- Shortness of breath
- Fast breathing
- Hard breathing
- Paleness
- Failure to gain weight
- Fast heart rate
- Sweating while feeding
- Frequent respiratory infections
Exams and Tests
Listening with a stethoscope most often reveals a heart murmur. The loudness of the murmur is related to the size of the defect and amount of blood crossing the defect.
Tests may include:
- Cardiac catheterization (rarely needed, unless there are concerns of high blood pressure in the lungs)
- Chest x-ray -- looks to see if there is a large heart with fluid in the lungs
- ECG -- shows signs of an enlarged left ventricle
- Echocardiogram -- used to make a definite diagnosis
- MRI or CT scan of the heart -- used to see the defect and find out how much blood is getting to the lungs
Treatment
If the defect is small, no treatment may be needed. But the baby should be closely monitored by a health care provider. This is to make sure that the hole eventually closes properly, and signs of heart failure do not occur.
Babies with a large VSD who have symptoms related to heart failure may need medicine to control the symptoms and surgery to close the hole. Diuretic medicines are often used to relieve symptoms of congestive heart failure.;
If symptoms continue, even with medicine, surgery to close the defect with a patch is needed. Some VSDs can be closed with a special device during a cardiac catheterization, which avoids the need for surgery. This is called transcatheter closure. However, only certain types of defects can successfully be treated this way.
Having surgery for a VSD with no symptoms is controversial, especially when there is no evidence of heart damage. Discuss this carefully with your provider.
Outlook (Prognosis)
Many small defects will close on their own. Surgery can repair defects that do not close. In most cases, a person will not have any ongoing medical issues related to the defect if it is closed with surgery or closes on its own. Complications may occur if a large defect is not treated and there is permanent damage to the lungs.
Possible Complications
Complications may include:
- Aortic insufficiency (leaking of the valve that separates the left ventricle from the aorta)
- Damage to the electrical conduction system of the heart during surgery (causing an irregular or slow heart rhythm)
- Delayed growth and development (failure to thrive in infancy)
- Heart failure
- Infective endocarditis (bacterial infection of the heart)
- Pulmonary hypertension (high blood pressure in the lungs) leading to failure of the right side of the heart
When to Contact a Medical Professional
Most often, this condition is diagnosed during a routine exam of an infant. Contact your infant's provider if the baby seems to be having trouble breathing, or if the baby seems to have an unusual number of respiratory infections.
Prevention
Except for a VSD that is caused by a heart attack, this condition is always present at birth.
Drinking alcohol and using the antiseizure medicines valproic acid (Depakote) and phenytoin (Dilantin) during pregnancy may increase the risk for VSDs. Other than avoiding these things during pregnancy, there is no known way to prevent a VSD.
Women who plan to become pregnant should be immunized against rubella if they are not already immune. Rubella infection in a pregnant woman can cause congenital heart disease.
Women who are pregnant should get good prenatal care:
- Avoid alcohol and illegal drugs during pregnancy.
- Tell your provider that you are pregnant before taking any new medicines.
- Have a blood test early in your pregnancy to see if you are immune to rubella. If you are not immune, avoid any possible exposure to rubella and get vaccinated right after delivery.
- Pregnant women who have diabetes should try to get good control over their blood sugar level.
Related Information
Heart failureAortic regurgitation
Arrhythmias
Delayed growth
Failure to thrive
Pediatric heart surgery
Pediatric heart surgery - discharge
References
Valente AM, Dorfman AL, Babu-Narayan SV, Kreiger EV. Congenital heart disease in the adolescent and adult. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 82.
Well A, Fraser CD. Congenital heart disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 59.
BACK TO TOPReview Date: 10/23/2023
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
