Gestational diabetes
Glucose intolerance during pregnancy
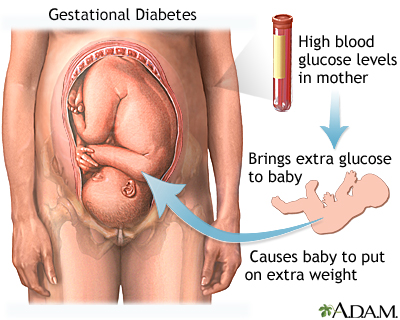
Gestational diabetes is high blood sugar (glucose) that starts or is first diagnosed during pregnancy.
Images
Causes
Pregnancy hormones can inhibit insulin from doing its job. When this happens, glucose level may increase in a pregnant woman's blood.
You are at greater risk for gestational diabetes if you:
- Are older than 25 when you are pregnant
- Come from a higher risk ethnic group, such as Latino, African American, Native American, Asian, or Pacific Islander
- Have a family history of diabetes
- Gave birth to a baby that weighed more than 9 pounds (4 kg) or had a birth defect
- Have high blood pressure
- Have too much amniotic fluid
- Have had an unexplained miscarriage or stillbirth
- Were overweight before your pregnancy
- Gain too much weight during your pregnancy
- Have polycystic ovary syndrome
Symptoms
Most of the time, there are no symptoms. The diagnosis is made during a routine prenatal screening.
Mild symptoms, such as increased thirst or shakiness, may be present. These symptoms are usually not dangerous to the pregnant woman.
Other symptoms may include:
- Blurred vision
- Fatigue
- Frequent infections, including those of the bladder, vagina, and skin
- Increased thirst
- Increased urination
Exams and Tests
Gestational diabetes most often starts halfway through the pregnancy. All pregnant women should receive an oral glucose tolerance test (glucose challenge test) between the 24th and 28th week of pregnancy to look for the condition. Some women who have a low risk of gestational diabetes may skip this test but should always ask their health care provider what is best for them. Women who have risk factors for gestational diabetes may have this test earlier in the pregnancy.
Once you are diagnosed with gestational diabetes, you can see how well you are doing by testing your glucose level at home. The most common way involves pricking your finger and putting a drop of your blood on a machine that will give you a glucose reading.
Treatment
The goals of treatment are to keep blood sugar (glucose) level within normal limits during the pregnancy, and to make sure that the growing baby is healthy.
WATCHING YOUR BABY
Your provider should closely check both you and your baby throughout your pregnancy. Fetal monitoring will check the size and health of your baby.
A nonstress test is a very simple, painless test for you and your baby.
- A machine that hears and displays your baby's heartbeat (electronic fetal monitor) is placed on your abdomen.
- Your provider can compare the pattern of your baby's heartbeat to movements and find out whether the baby is doing well.
If you take medicine to control diabetes, you may need to be monitored more often toward the end of your pregnancy.
DIET AND EXERCISE
In many cases, eating healthy foods, staying active, and managing your weight are all that are needed to treat gestational diabetes.
The best way to improve your diet is by eating a variety of healthy foods. You should learn how to read food labels and check them when making food decisions. Talk to your provider if you are a vegetarian or on another special diet.
In general, when you have gestational diabetes, your diet should:
- Be moderate in fat and protein
- Provide carbohydrates through foods that include fruits, vegetables, and complex carbohydrates (such as bread, cereal, pasta, and rice)
- Be low in foods that contain a lot of sugar, such as soft drinks, fruit juices, and pastries
Talk with your provider about the physical activities that are right for you. Low-impact exercises, such as swimming, brisk walking, or using an elliptical machine are safe ways to control your blood sugar and weight.
If managing your diet and exercising don't control your blood sugar, you may be prescribed diabetes medicine or insulin therapy.
Outlook (Prognosis)
There are many risks of having diabetes in pregnancy when blood sugar is not well controlled. With good control, most pregnancies have good outcomes.
Pregnant women with gestational diabetes tend to have larger babies at birth. This can increase the chance of problems at the time of delivery, including:
- Birth injury (trauma) because of the baby's large size
- Delivery by C-section
Your baby is more likely to have periods of low blood sugar (hypoglycemia) during the first few days of life, and may need to be monitored in a neonatal intensive care unit (NICU) for a few days.
Mothers with gestational diabetes have an increased risk for high blood pressure during pregnancy and increased risk for preterm delivery. Mothers with seriously uncontrolled blood sugar have a higher risk for stillbirth.
After delivery:
- Your high blood sugar (glucose) level often goes back to normal.
- You should be closely followed for signs of diabetes over the next 5 to 10 years after delivery.
When to Contact a Medical Professional
Contact your provider if you are pregnant and you have symptoms of diabetes.
Prevention
Early prenatal care and having regular checkups helps improve your health and the health of your baby. Getting prenatal screening at 24 to 28 weeks of pregnancy will help detect gestational diabetes early.
If you are overweight, getting your weight within the normal body mass index (BMI) range will decrease your risk for gestational diabetes.
Related Information
CarbohydratesBlood sugar test
Overweight
Low blood sugar
References
American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S158-S178. PMID: 38078590 pubmed.ncbi.nlm.nih.gov/38078590/.
Egan AM, Dinneen SF. Classification and diagnosis of diabetes mellitus. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 137.
Landon MB, Catalano PM, Gabbe SG. Diabetes mellitus complicating pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 45.
US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for gestational diabetes: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326(6):531-538. PMID: 34374716 pubmed.ncbi.nlm.nih.gov/34374716/.
BACK TO TOPReview Date: 4/16/2024
Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
