Bell palsy
Facial palsy; Idiopathic peripheral facial palsy; Cranial mononeuropathy - Bell palsy; Bell's palsy
Bell palsy is a disorder of the nerve that controls movement of the muscles in the face. This nerve is called the facial or seventh cranial nerve.
Damage to this nerve causes weakness or paralysis of these muscles. Paralysis means that you cannot use the muscles at all.
Images
Causes
Bell palsy can affect people of any age, most commonly those over age 65 years. It can also affect children younger than 10 years. Males and females are equally affected.
Bell palsy is thought to be due to swelling (inflammation) of the facial nerve in the area where it travels through the bones of the skull. This nerve controls movement of the muscles of the face.
The cause is often not clear. A type of herpes infection called herpes simplex or herpes zoster might be involved. Other conditions that may affect the seventh cranial nerve include:
- HIV/AIDS infection
- Lyme disease
- Middle ear infection
- Sarcoidosis (inflammation of the lymph nodes, lungs, liver, eyes, skin, or other tissues)
Having diabetes and being pregnant may increase the risk for Bell palsy.
Symptoms
Sometimes, you may have a cold shortly before the symptoms of Bell palsy begin.
Symptoms most often start suddenly, but may take 2 to 3 days to become fully developed. They do not become more severe after that.
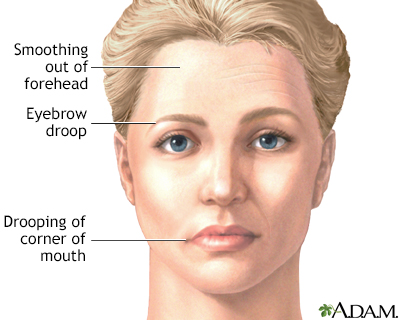
Symptoms are almost always on one side of the face only. They may range from mild to severe.
Many people feel discomfort behind the ear before weakness is noticed. The face feels stiff or pulled to one side and may look different. Other signs can include:
- Difficulty closing one eye
- Difficulty eating and drinking because food falls out of one side of the mouth
- Drooling due to lack of control over the muscles of the face
- Slurring your words (dysarthria) due to lip weakness
- Drooping of the face, such as the eyelid or corner of the mouth
- Problems smiling, grimacing, or making facial expressions
- Twitching or weakness of the muscles in the face
Other symptoms that may occur:
- Dry eye, which may lead to eye sores or infections
- Dry mouth
- Headache if there is an infection such as Lyme disease
- Loss of sense of taste
- Sound that is louder in one ear (hyperacusis)
Exams and Tests
Often, Bell palsy can be diagnosed just by taking a health history and doing a complete physical exam.
Blood tests may be done to look for medical problems such as Lyme disease, which may cause Bell palsy.
Sometimes, a test is needed to check the nerves that supply the muscles of the face:
- Electromyography (EMG) to check the health of the facial muscles and the nerves that control the muscles
- Nerve conduction test to check how fast electrical signals move through a nerve
If your health care provider is worried there is another cause for your symptoms, they may suggest:
Treatment
Often, no treatment is needed. Symptoms often begin to improve right away. But, it may take weeks or even months for the muscles to get stronger.
Your provider may give you lubricating eye drops or eye ointments to keep the surface of the eye moist if you can't close it completely. You may need to wear an eye patch while you sleep.
Often, medicines may be used to improve the chances of recovery, but they must be started right away. Common medicines are:
- Corticosteroids, which may reduce swelling around the facial nerve
- Medicines such as valacyclovir to fight the virus that may be causing Bell palsy
Surgery to relieve pressure on the nerve (decompression surgery) has not been shown to benefit most people with Bell palsy.
Outlook (Prognosis)
Most cases go away completely within a few weeks to months.
If you did not lose all of your nerve function and symptoms began to improve within 3 weeks, you are more likely to regain all or most of the strength in your facial muscles.
Sometimes, the following symptoms may still be present:
- Long-term changes in taste
- Spasms of muscles or eyelids
- Weakness that remains in facial muscles
Possible Complications
Complications may include:
- Eye surface becoming dry, leading to eye sores, infections, and vision loss
- Swelling in the muscles due to loss of nerve function
When to Contact a Medical Professional
Contact your provider right away if your face droops or you have other symptoms of Bell palsy. Your provider can rule out other, more serious conditions, such as stroke.
Prevention
There is no known way to prevent Bell palsy.
Related Information
Facial paralysisAcute
Peripheral neuropathy
Incidence
Mononeuropathy
Head injury - first aid
Tumor
Corneal ulcers and infections
Chronic
References
National Institute of Neurological Disorders and Stroke website. Bell's palsy. www.ninds.nih.gov/health-information/disorders/bells-palsy. Updated May 2, 2024. Accessed July 1, 2024.
Ryan MM. Bell palsy. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 657.
Smith G, Shy ME. Peripheral neuropathies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 388.
Wallenstein J. Brain and cranial nerve disorders. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 91.
BACK TO TOPReview Date: 6/13/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
