Brain tumor - children
Glioblastoma multiforme - children; Ependymoma - children; Glioma - children; Astrocytoma - children; Medulloblastoma - children; Neuroglioma - children; Oligodendroglioma - children; Meningioma - children; Cancer - brain tumor (children)
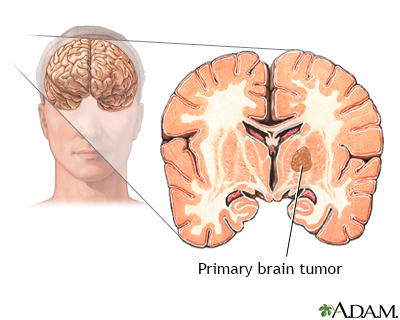
A brain tumor is a group (mass) of abnormal cells that grow in the brain.
This article focuses on primary brain tumors in children.
Images
Causes
The cause of primary brain tumors is often unknown. Some primary brain tumors are related to other syndromes or can run in a family. They can be:
- Not cancerous (benign)
- Invasive (spread to nearby areas)
- Cancerous (malignant)
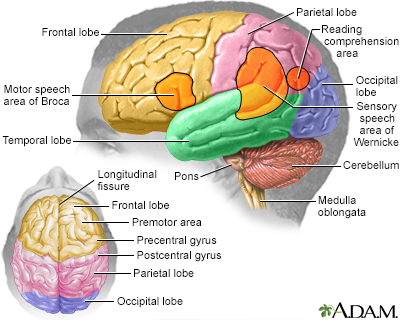
Brain tumors are classified based on:
- The exact site of the tumor
- The type of tissue involved
- Whether it is cancerous
Brain tumors can directly kill brain cells. They can also damage cells by pushing on other parts of the brain. This leads to swelling and increased pressure inside the skull.
Tumors can occur at any age. Many tumors are more common at a certain age. In general, brain tumors in children are very rare.
COMMON TUMOR TYPES
Astrocytomas are usually noncancerous, slow-growing tumors. They most often develop in children ages 5 to 8. Also called low-grade gliomas, these are the most common brain tumors in children.
Medulloblastomas are the most common type of childhood brain cancer. Most medulloblastomas occur before age 10.
Ependymomas are a type of childhood brain tumor that can be benign or malignant. Therapy to control the tumor is based on the location and type of ependymoma.
Brainstem gliomas are very rare tumors that occur almost only in children. The average age at which they develop in children is about age 6.
Symptoms
Symptoms may be subtle and slowly become worse, or they may occur very quickly.
Headaches are often the most common symptom. But only very rarely do children with headaches have a tumor. Headache patterns that may occur with brain tumors include:
- Headaches that are worse when waking up in the morning and go away within a few hours
- Headaches that get worse with coughing or exercise, or with a change in body position
- Headaches that occur while sleeping and with at least one other symptom such as vomiting or confusion
Sometimes, the only symptoms of brain tumors are mental changes, which may include:
- Changes in personality and behavior
- Unable to concentrate
- Increased sleep
- Memory loss
- Problems with reasoning
Other possible symptoms are:
- Seizures
- Unexplained frequent vomiting
- Gradual loss of movement or feeling in an arm or leg
- Hearing loss with or without dizziness
- Speech difficulty
- Unexpected vision problem (if it occurs with a headache), including vision loss (peripheral vision) in one or both eyes, or double vision
- Problems with balance
- Weakness or numbness
Exams and Tests
The health care provider will perform a physical exam. Infants may have the following physical signs:
- Bulging fontanelle
- Enlarged eyes
- No red reflex in the eye
- Positive Babinski reflex
- Separated sutures of the skull bones
Older children with brain tumors may have the following physical signs or symptoms:
- Headache
- Vomiting
- Vision changes
- Change how the child walks (gait)
- Weakness of a specific body part
- Head tilt
The following tests may be used to detect a brain tumor and identify its location:
Treatment
Treatment depends on the size and type of tumor and the child's general health. The goals of treatment may be to cure the tumor, relieve symptoms, and improve brain function or the child's comfort.
Surgery is needed for most primary brain tumors. Some tumors may be completely removed. In cases where the tumor can't be removed, surgery may help reduce pressure and relieve symptoms. Chemotherapy or radiation therapy may be used for certain tumors.
The following are treatments for specific types of tumors:
- Astrocytoma: Surgery to remove the tumor is the main treatment. Chemotherapy or radiation therapy may also be needed.
- Brainstem gliomas: Surgery may not be possible because of the tumor's location deep in the brain. Radiation is used to shrink the tumor and prolong life. Sometimes targeted chemotherapy can be used.
- Ependymomas: Treatment includes surgery. Radiation and chemotherapy may be necessary.
- Medulloblastomas: Surgery alone does not cure this type of tumor. Chemotherapy with or without radiation is often used in combination with surgery.
Medicines used to treat children with primary brain tumors include:
- Corticosteroids to reduce brain swelling
- Diuretics (water pills) to reduce brain swelling and pressure
- Anticonvulsants to reduce or prevent seizures
- Pain medicines
- Chemotherapy to help shrink the tumor or prevent the tumor from growing back
Comfort measures, safety measures, physical therapy, occupational therapy, and other such steps may be required to improve quality of life.
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you and your child feel less alone.
Outlook (Prognosis)
How well a child does depends on many things, including the type of tumor. In general, about 3 out of 4 children survive at least 5 years after being diagnosed.
Long-term brain and nervous system problems may result from the tumor itself or from treatment. Children may have problems with attention, focus, or memory. They may also have problems processing information, planning, insight, or initiative or desire to do things.
Children younger than age 7, especially younger than age 3, seem to be at greatest risk of these complications.
Parents need to make sure that children receive support services at home and at school.
When to Contact a Medical Professional
Contact a provider if a child develops headaches that do not go away or other symptoms of a brain tumor.
Go to the emergency room if a child develops any of the following:
- Physical weakness
- Change in behavior
- Severe headache of unknown cause
- Seizure of unknown cause
- Vision changes
- Speech changes
Related Information
Metastatic brain tumorBrain tumor - primary - adults
Tumor
Invasive
Benign
Malignancy
Increased intracranial pressure
Central nervous system
Headache
Nausea and vomiting – adults
Radiation therapy
Chemotherapy
Movement - uncoordinated
Fatigue
Vision problems
Walking abnormalities
Endocrine glands
Brain herniation
Proton therapy
Brain surgery
Chemotherapy - what to ask your doctor
Radiation therapy - questions to ask your doctor
Brain radiation - discharge
Brain surgery - discharge
References
Kieran MW, Chi SN, Manley PE, et al. Tumors of the brain and spinal cord. In: Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux SE, Nathan DG, eds. Nathan and Oski's Hematology and Oncology of Infancy and Childhood. 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 57.
National Cancer Institute website. Childhood brain and spinal cord tumors treatment overview (PDQ): health professional version. www.cancer.gov/types/brain/hp/child-brain-treatment-pdq. Updated October 8, 2021. Accessed September 9, 2023.
Zaky W, Ater JL, Khatua S. Brain tumors in childhood. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 524.
BACK TO TOPReview Date: 8/28/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
