Drug-induced immune hemolytic anemia
Immune hemolytic anemia secondary to drugs; Anemia - immune hemolytic - secondary to drugs
Drug-induced immune hemolytic anemia is a blood disorder that occurs when a medicine triggers the body's defense (immune) system to attack its own red blood cells. This causes red blood cells to break down earlier than normal, a process called hemolysis.
Images
I Would Like to Learn About:
Causes
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
Normally, red blood cells last for about 120 days in the body. In people with hemolytic anemia, red blood cells in the blood are destroyed earlier than normal.
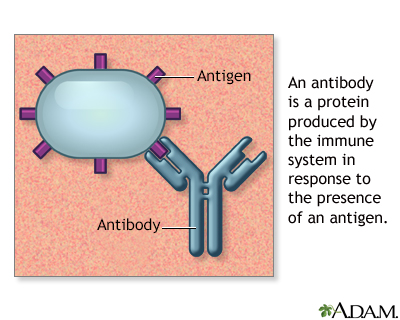
In some cases, a drug can cause the immune system to mistake your own red blood cells for foreign substances. The body responds by making antibodies to attack the body's own red blood cells. The antibodies attach to red blood cells and cause them to break down too early.
Drugs that can cause this type of hemolytic anemia include:
- Cephalosporins (a class of antibiotics), most common cause
- Dapsone
- Levodopa
- Levofloxacin
- Methyldopa
- Nitrofurantoin
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Penicillin and its derivatives
- Phenazopyridine (Pyridium)
- Quinidine
Drug-induced hemolytic anemia is rare in children.
Symptoms
Symptoms may include any of the following:
- Dark urine
- Fatigue
- Pale skin color
- Rapid heart rate
- Shortness of breath
- Yellow skin and whites of the eyes (jaundice)
Exams and Tests
A physical exam may show an enlarged spleen. You may have blood and urine tests to help diagnose this condition.
Tests may include:
- Absolute reticulocyte count to determine if red blood cells are being created in the bone marrow at an appropriate rate
- Direct or indirect Coombs test to check if there are antibodies against red blood cells that are causing red blood cells to die too early
- Indirect bilirubin levels to check for jaundice
- Red blood cell count
- Serum haptoglobin to check if red blood cells are being destroyed too early
- Lactate dehydrogenase level, which increases with red cell destruction
- Urine hemoglobin to check for hemolysis
Treatment
Stopping the drug that is causing the problem may relieve or control the symptoms.
You may need to take a medicine called prednisone to suppress the immune response against the red blood cells. Special blood transfusions may be needed to treat severe symptoms.
Outlook (Prognosis)
The outcome is good for most people if they stop taking the drug that is causing the problem.
Possible Complications
Death caused by severe anemia is rare.
When to Contact a Medical Professional
See your health care provider if you have symptoms of this condition.
Prevention
Avoid the drug that caused this condition.
Related Information
Hemolytic anemiaAntibody
Glucose-6-phosphate dehydrogenase deficiency
Hemolytic transfusion reaction
References
Brandow AM. Hemolytic anemias resulting from extracellular factors -- immune hemolytic anemias. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 491.
Michel M. Autoimmune and intravascular hemolytic anemias. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 151.
BACK TO TOPReview Date: 2/2/2023
Reviewed By: Mark Levin, MD, Hematologist and Oncologist, Monsey, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
