Type 1 diabetes
Insulin-dependent diabetes; Juvenile onset diabetes; Diabetes - type 1; High blood sugar - type 1 diabetes
Type 1 diabetes is a lifelong (chronic) disease in which there is a high level of sugar (glucose) in the blood.
Images

Causes
Type 1 diabetes can occur at any age. It is most often diagnosed in children, adolescents, or young adults.
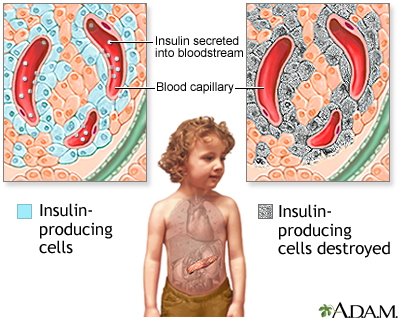
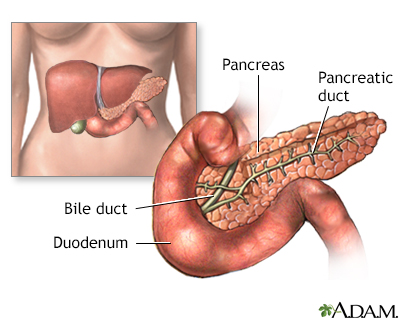
Insulin is a hormone produced in the pancreas by special cells, called beta cells. The pancreas is below and behind the stomach. Insulin is needed to move glucose into cells. Inside the cells, glucose is stored and later used for energy. With type 1 diabetes, beta cells produce little or no insulin.
Without enough insulin, glucose builds up in the bloodstream instead of going into the cells. This buildup of glucose in the blood is called hyperglycemia. The body is unable to use the glucose for energy. This leads to the symptoms of type 1 diabetes.
The exact cause of type 1 diabetes is unknown. It is an autoimmune disorder. This is a condition that occurs when the immune system mistakenly attacks and destroys healthy body tissue. In people with type 1 diabetes, an infection or another trigger causes the body to mistakenly attack the beta cells in the pancreas that make insulin. The tendency to develop autoimmune diseases, including type 1 diabetes, can be inherited from your parents.
Symptoms
HIGH BLOOD SUGAR
The following symptoms may be the first signs of type 1 diabetes. Or, they may occur when blood sugar is high.
- Being very thirsty
- Feeling hungry
- Feeling tired all the time
- Having blurry eyesight
- Feeling numbness or tingling in your feet
- Losing weight despite an increased appetite
- Urinating more often (including urinating at night or bedwetting in children who were dry overnight before)
For other people, these serious warning symptoms may be the first signs of type 1 diabetes. Or, they may happen when blood sugar is very high (diabetic ketoacidosis):
- Deep, rapid breathing
- Dry skin and mouth
- Flushed face
- Fruity breath odor
- Nausea and vomiting; inability to keep down fluids
- Stomach pain
LOW BLOOD SUGAR
Low blood sugar (hypoglycemia) can develop quickly in people with diabetes who are taking insulin. Symptoms usually appear when a person's blood sugar level falls below 70 milligrams per deciliter (mg/dL), or 3.9 millimoles per liter (mmol/L). Watch for:
- Headache
- Hunger
- Nervousness, irritability
- Rapid heartbeat (palpitations)
- Shaking
- Sweating
- Weakness
After many years, diabetes can lead to serious health problems, and as a result, many other symptoms.
Exams and Tests
Diabetes is diagnosed with the following blood tests:
- Fasting blood glucose level -- Diabetes is diagnosed if it is 126 mg/dL (7 mmol/L) or higher two different times while in the usual state of health.
- Random (non-fasting) blood glucose level -- You may have diabetes if it is 200 mg/dL (11.1 mmol/L) or higher. (This must be confirmed with a fasting test.)
- Oral glucose tolerance test -- Diabetes is diagnosed if the glucose level is 200 mg/dL (11.1 mmol/L) or higher 2 hours after you drink a special sugar drink.
- Hemoglobin A1C (A1C) test -- Diabetes is diagnosed if the result of the test is 6.5% or higher.
Ketone testing is also used sometimes. The ketone test is done using a urine sample or blood sample. Ketone testing may be done to determine if someone with type 1 diabetes has had ketoacidosis. Testing is usually done:
- When the blood sugar is higher than 240 mg/dL (13.3 mmol/L)
- During an illness such as pneumonia, heart attack, or stroke
- When nausea and vomiting occur
- During pregnancy
The following exams and tests will help you and your health care provider monitor your diabetes and prevent problems caused by diabetes:
- Check the skin and bones on your feet and legs.
- Check if your feet are getting numb (diabetic nerve disease).
- Have your blood pressure checked at least once a year. The goal should be lower than 130/80 millimeters of mercury (mmHg).
- Have an A1C test done every 6 months if your diabetes is well controlled. Have the test done every 3 months if your diabetes is not well controlled.
- Have your cholesterol and triglyceride levels checked once a year.
- Get tests once a year to make sure your kidneys are working well. These tests include checking levels of urine albumin (microalbuminuria) and serum creatinine.
- Visit your eye doctor at least once a year, or more often if you have signs of diabetic eye disease, once you have had type 1 diabetes for 5 years.
- See your dentist every 6 months for a thorough dental cleaning and exam. Make sure your dentist and hygienist know that you have diabetes.
Treatment
Because type 1 diabetes can start quickly and the symptoms can be severe, people who have just been diagnosed may need to stay in the hospital.
If you have just been diagnosed with type 1 diabetes, you may need to have a checkup each week until you have good control over your blood sugar. Your provider will review the results of your home blood sugar monitoring and urine testing. Your provider will also look at your diary of meals, snacks, and insulin injections. It may take a few weeks to match the insulin doses to your meal and activity schedules.
As your diabetes becomes more stable, you will have fewer follow-up visits. Visiting your provider is very important so you can monitor any long-term problems from diabetes.
Your provider will likely ask you to meet with a dietitian, clinical pharmacist, and certified diabetes care and education specialist (CDCES). These providers will also help you manage your diabetes.
But, you are the most important person in managing your diabetes. You should know the basic steps of diabetes management, including:
- How to recognize and treat low blood sugar (hypoglycemia)
- How to recognize and treat high blood sugar (hyperglycemia)
- How to plan meals, including carbohydrate (carb) counting
- How to give insulin
- How to check blood glucose and urine ketones
- How to adjust insulin and food when you exercise
- How to handle sick days
- Where to buy diabetes supplies and how to store them
INSULIN
Insulin lowers blood sugar by allowing it to leave the bloodstream and enter cells. Everyone with type 1 diabetes must take insulin every day.
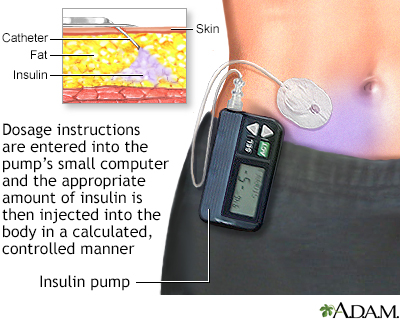
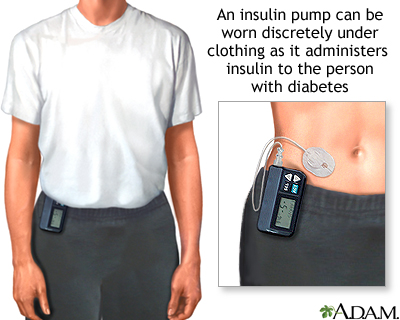
Most commonly, insulin is injected under the skin using a syringe, insulin pen, or insulin pump. Another form of insulin is the inhaled type. Insulin cannot be taken by mouth because the acid in the stomach destroys insulin.
Insulin types differ in how fast they start to work and how long they last. Your provider will choose the best type of insulin for you and will tell you at what time of day to use it. Some types of insulin may be mixed together in an injection to get the best blood glucose control. Other types of insulin should never be mixed.
Most people with type 1 diabetes need to take two kinds of insulin. Basal insulin is long-lasting and controls how much sugar your own body makes when you are not eating. Meal-time (bolus or prandial) insulin is rapid acting and is taken with every meal, usually a few minutes before you start eating. It lasts only long enough to help move the sugar absorbed from a meal into muscle and fat cells for storage.
Your provider or diabetes educator will teach you how to give insulin injections. At first, a child's injections may be given by a parent or another adult. By age 14, most children can give themselves their own injections.
Inhaled insulin comes as a powder that is breathed in (inhaled). It is rapid acting and used just before each meal. Your provider can tell you if this type of insulin is right for you.
People with diabetes need to know how to adjust the amount of insulin they are taking:
- When they exercise
- When they are sick
- When they will be eating more or less food and calories
- When they are traveling
HEALTHY EATING AND EXERCISE
By testing your blood sugar level, you can learn which foods and activities raise or lower your blood sugar level the most. This helps you adjust your insulin doses to specific meals or activities to prevent blood sugar from becoming too high or too low.
The American Diabetes Association and the Academy of Nutrition and Dietetics have information for planning healthy, balanced meals. It also helps to talk to a registered dietitian or nutrition counselor.
Regular exercise helps control the amount of sugar in the blood. It also helps burn extra calories and fat to reach and maintain a healthy weight.
Talk to your provider before starting any exercise program. People with type 1 diabetes must take special steps before, during, and after physical activity or exercise.
MANAGING YOUR BLOOD SUGAR
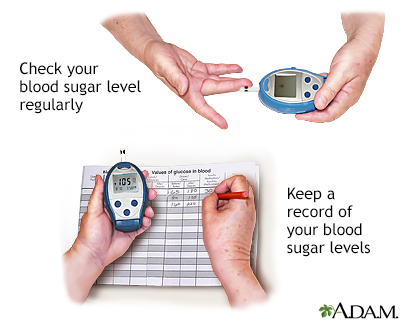
Checking your blood sugar level yourself and recording the results tells you how well you are managing your diabetes. Talk to your provider and diabetes educator about how often to check.
To check your blood sugar level, you may use a device called a glucose meter. Usually, you prick your finger with a small needle, called a lancet, to get a tiny drop of blood. You place the blood on a test strip and put the strip into the meter. The meter gives you a reading that tells you the level of your blood sugar.
A continuous glucose monitor (CGM) estimates your blood sugar level from fluid under your skin. These monitors are used mostly by people who also use insulin pumps to control their diabetes but they are often helpful for people not using an insulin pump. Most monitors do not require a finger prick.
Keep a record of your blood sugar for yourself and your health care team. This can often be done most easily using a website designed for this purpose. These numbers will help if you have problems managing your diabetes. You and your provider should set a target goal for your blood sugar level at different times during the day. You should also plan what to do when your blood sugar is too low or high.
Talk to your provider about your target for the A1C test. This lab test shows your average blood sugar level over the past 3 months. It shows how well you are controlling your diabetes. For most people with type 1 diabetes, the A1C target should be 7% or lower.
Low blood sugar is called hypoglycemia. A blood sugar level below 70 mg/dL (3.9 mmol/L) is too low and can harm you. A blood sugar level below 54 mg/dL (3.0 mmol/L) is cause for immediate action. Keeping good control of your blood sugar can help prevent low blood sugar. Talk to your provider if you're not sure about the causes and symptoms of low blood sugar.
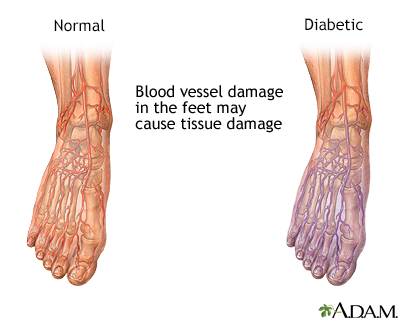
FOOT CARE
People with diabetes are more likely than those without diabetes to have foot problems. Diabetes damages the nerves. This can make your feet less able to feel pressure, pain, heat, or cold. You may not notice a foot injury until you have severe damage to the skin and tissue below, or you get a severe infection.
Diabetes can also damage blood vessels. Small sores or breaks in the skin may become deeper skin sores (ulcers). The affected limb may need to be amputated if these skin ulcers do not heal, or become larger, deeper, or infected.
To prevent problems with your feet:
- Stop using tobacco, if you use it.
- Improve control of your blood sugar.
- Get a foot exam at least once a year from your provider, and learn whether you have nerve damage.
- Ask your provider to check your feet for problems such as calluses, a bunion or hammertoe. These need to be treated to prevent skin breakdown and ulcers.
- Check and care for your feet every day. This is very important when you already have nerve or blood vessel damage or foot problems.
- Treat minor infections, such as athlete's foot, right away.
- Good nail care is important. If your nails are very thick and hard, you should have your nails trimmed by a podiatrist or other provider who knows you have diabetes.
- Use moisturizing lotion on dry skin.
- Make sure you wear the right kind of shoes. Ask your provider what kind is right for you.
PREVENTING COMPLICATIONS
Your provider may prescribe medicines or other treatments to reduce your chances of developing common complications of diabetes, including:
- Eye disease
- Kidney disease
- Peripheral nerve damage
- Heart disease and stroke
With type 1 diabetes, you are also at risk of developing conditions such as hearing loss, gum disease, bone disease, or yeast infections (in women). Keeping your blood sugar under good control can help prevent these conditions.
Talk with your health care team about other things you can do to lower your chances of developing diabetes complications.
People with diabetes should make sure to keep up on their vaccination schedule.
EMOTIONAL HEALTH
Living with diabetes is often stressful at times. You may feel overwhelmed by everything you need to do to manage your diabetes. But taking care of your emotional health is just as important as your physical health.
Ways to relieve stress include:
- Listening to relaxing music
- Meditating to take your mind off your worries
- Deep breathing to help relieve physical tension
- Doing yoga, tai chi, or progressive relaxation
Feeling sad or down (depressed) or anxious sometimes is normal. But if you have these feelings often and they're getting in the way of managing your diabetes, talk with your health care team. They can find ways to help you feel better.
Support Groups
There are many diabetes resources that can help you understand more about type 1 diabetes. You can also learn ways to manage your condition so that you can live well with diabetes.
More information and support for people with diabetes and their families can be found at :
- American Diabetes Association -- www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases -- www.niddk.nih.gov/health-information/diabetes
Outlook (Prognosis)
Type 1 diabetes is a lifelong disease and there is no cure.
Tight control of blood glucose can prevent, delay, and minimize diabetes complications. But these problems can occur, even in people with good diabetes control.
Possible Complications
After many years, diabetes can lead to serious health problems:
- You could have eye problems, including trouble seeing (especially at night), cataracts, and sensitivity to light. You could become blind.
- Your feet and skin could develop sores and infections. If you have these sores for too long, your foot or leg may need to be amputated. Infection can also cause pain, swelling, and itching.
- Diabetes may make it harder to control your blood pressure and cholesterol. This can lead to heart attack, stroke, and other problems. It can become harder for blood to flow to your legs and feet.
- Nerves in your body can become damaged, causing pain, itching, tingling, and numbness.
- Because of nerve damage, you could have problems digesting the food you eat. You could feel weakness or have trouble going to the bathroom. Nerve damage can also make it harder for men to have an erection.
- High blood sugar and other problems can lead to kidney damage. The kidneys may not work as well as they used to. They may even stop working, so that you would need dialysis or a kidney transplant.
- High blood sugar can weaken your immune system. This may make it more likely for you to get infections, including life-threatening skin and fungal infections.
When to Contact a Medical Professional
Call 911 or the local emergency number if you have:
- Chest pain or pressure, shortness of breath, or other signs of angina
- Loss of consciousness
- Seizures
- Shortness of breath
- Red, painful skin that is spreading quickly
Contact your provider or go to the emergency room if you have symptoms of diabetic ketoacidosis.
Also contact your provider if you have:
- Blood sugar levels that are higher than the goals you and your provider have set
- Numbness, tingling, or pain in your feet or legs
- Problems with your eyesight
- Sores or infections on your feet
- Frequent feelings of depression or anxiety
- Symptoms that your blood sugar is getting too low (weakness or fatigue, trembling, sweating, irritability, trouble thinking clearly, fast heartbeat, double or blurry vision, uneasy feeling)
- Symptoms that your blood sugar is too high (thirst, blurry vision, dry skin, weakness or fatigue, need to urinate a lot)
- Blood sugar readings that are below 70 mg/dL (3.9 mmol/L)
You can treat early signs of hypoglycemia at home by drinking orange juice, eating sugar or candy, or by taking glucose tablets. You can follow the rule of 15, which advises eating 15 grams of fast-acting carbohydrates and then rechecking your blood sugar in 15 minutes to ensure resolution. If signs of hypoglycemia continue or your blood glucose level stays below 60 mg/dL (3.3 mmol/L), go to the emergency room.
Prevention
Type 1 diabetes cannot be prevented currently. This is a very active area of research. In 2019, a study using an injectable medicine was able to delay the onset of type 1 diabetes in high-risk children. There is no screening test for type 1 diabetes in people who have no symptoms. However, antibody testing can identify people at higher risk of developing type 1 diabetes if they have first-degree relatives (sibling, parent) with type 1 diabetes or if you have symptoms and would like further testing.
Related Information
Type 2 diabetesGestational diabetes
Carbohydrates
Protein in diet
Diabetes and eye disease
Retinal detachment
Iris
Glaucoma
Cataract - adult
Acute kidney failure
Urinary tract infection - adults
Injury - kidney and ureter
Diabetes and nerve damage
Arterial insufficiency
Bunions
Leg or foot amputation
Foot amputation - discharge
Leg amputation - discharge
Leg or foot amputation - dressing change
Diabetes - foot ulcers
Diabetes eye care
Diabetes - when you are sick
Diabetes - preventing heart attack and stroke
Diabetes - taking care of your feet
Diabetes tests and checkups
Diabetes and exercise
Diabetes - keeping active
Low blood sugar - self-care
Managing your blood sugar
References
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in diabetes-2025. Diabetes Care. 2025;48(Supplement_1):S27-S49. PMID: 39651986 pubmed.ncbi.nlm.nih.gov/39651986/.
American Diabetes Association Professional Practice Committee. 12. Retinopathy, neuropathy, and foot care: standards of care in diabetes-2025. Diabetes Care. 2025;48(Supplement_1):S252-S265. PMID: 39651973 pubmed.ncbi.nlm.nih.gov/39651973/.
Brownlee M, Aiello LP, Sun JK, et al. Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Rosen CJ, Kopp PA, eds. Williams Textbook of Endocrinology.15th ed. Philadelphia, PA: Elsevier; 2025:chap 38.
Gillard P, Atkinson MA, Mathieu C. Type1 diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Rosen CJ, Kopp PA, eds. Williams Textbook of Endocrinology. 15th ed. Philadelphia, PA: Elsevier; 2025:chap 35.
BACK TO TOPReview Date: 1/10/2025
Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2025 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
