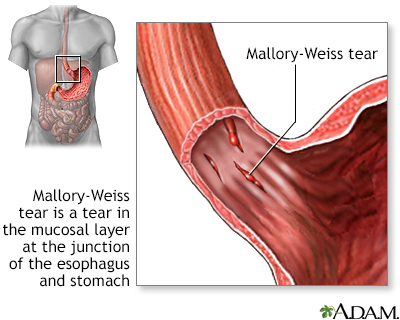
Mallory-Weiss tear
Mucosal lacerations - gastroesophageal junction
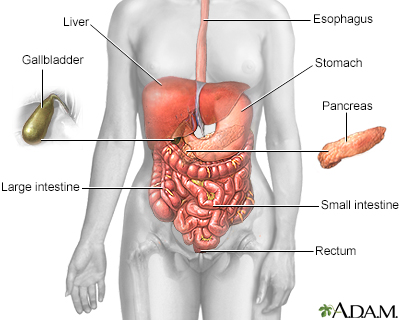
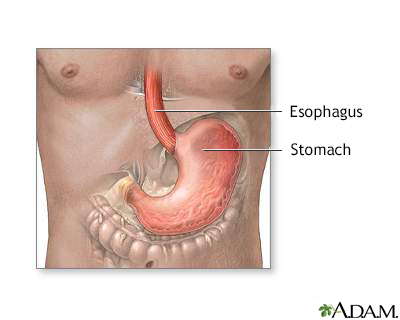
A Mallory-Weiss tear occurs in the mucous membrane of the lower part of the esophagus or upper part of the stomach, near where they join. The tear may bleed.
Images
Causes
Mallory-Weiss tears are most often caused by forceful or long-term vomiting or coughing. They may also be caused by epileptic convulsions.
Any condition that leads to violent and lengthy bouts of coughing or vomiting can cause these tears.
Symptoms
Symptoms may include:
- Bloody stools
- Vomiting blood (bright red)
Exams and Tests
Tests may include:
- CBC, possibly showing low hematocrit
- Esophagogastroduodenoscopy (EGD), more likely to be done when there is active bleeding
Treatment
The tear usually heals in a few days without treatment. The tear may also be fixed by clips that are put in during an EGD. Surgery is rarely needed. Drugs that suppress stomach acid (proton pump inhibitors or H2 blockers) may be given, but it is not clear if they are helpful.
If blood loss has been large, blood transfusions may be needed. In most cases, bleeding stops without treatment within a few hours.
Outlook (Prognosis)
Repeated bleeding is uncommon and the outcome is most often good. Cirrhosis of the liver and problems with blood clotting make future bleeding episodes more likely to occur.
Possible Complications
Hemorrhage (loss of blood)
When to Contact a Medical Professional
Contact your health care provider if you begin vomiting blood or if you pass bloody stools.
Prevention
Treatments to relieve vomiting and coughing may reduce risk. Avoid excessive alcohol use.
Related Information
MucosaNausea and vomiting – adults
Cough
Seizures
Incidence
References
Falk GW, Katzka DA. Diseases of the esophagus. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 129.
Katzka DA. Esophageal disorders caused by medications, trauma, and infection. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 45.
BACK TO TOPReview Date: 11/3/2022
Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
