Arthritis
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis.
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis.

Animation

Animation

Animation

Illustration

Illustration

Illustration

Illustration

Illustration

Illustration

Illustration

Illustration
Illustration

Illustration
Arthritis - Animation
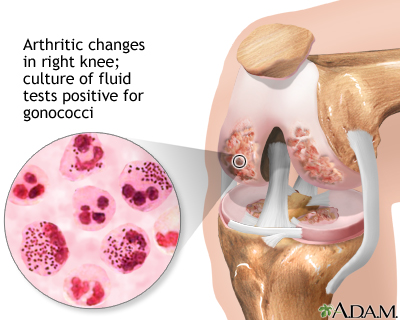
Arthritis, inflammation of one or more joints, is the most common cause of disability in the United States, limiting the activities of millions of adults. So, what causes arthritis? Cartilage, which is the tough but flexible tissue that covers the ends of your bones, normally protects and cushions a joint, allowing it to move smoothly. When this covering starts to break down, your bones rub together, causing pain, swelling, and stiffness. This is arthritis. Joint inflammation may result from an autoimmune disease like rheumatoid arthritis, which is when your immune system mistakenly attacks health tissue, or a broken bone, or general wear and tear on joints from osteoarthritis, or an infection from bacteria or a virus. If you have arthritis, you'll probably know it before you see your doctor. You may have joint pain, joint swelling, a reduced ability to move your joint, redness of the skin around your joint, and stiffness, especially in the morning. So, what do you do about arthritis? Your doctor will give you a physical exam and ask questions about your symptoms. Your doctor might find that you have fluid around a joint, warm, red, tender joints, and trouble moving your joints. You may have blood tests and x-rays to check for infection or other arthritis causes. Your doctor may take a sample of joint fluid with a needle and send it to a lab for examination. Once your doctor confirms that you have arthritis, your treatment will focus on reducing your pain, improving your mobility, and limiting further joint damage. Lifestyle changes are a big part of the treatment for arthritis. Exercise can help relieve stiffness, reduce pain and fatigue, and improve muscle and bone strength. Your health care team can help you design an exercise program that is best for you. Physical therapy may also be very helpful. You may use treatments like heat or ice, splints or orthotics to support your joints, water therapy, and even massage. You can take other steps to ease your pain. For example, sleeping 8 to 10 hours a night and taking naps during the day can help you recover from a flare-up more quickly, and may even help prevent them. Avoid staying in one position for too long, and avoid positions or movements that place extra stress on your joints. Install grab bars in the shower, tub, and near the toilet, to help you get around easier. Try stress reducing activities, such as meditation, yoga, or tai chi. Get more fruits, vegetables, cold water fish, and nuts into your diet. Weight loss through dieting and exercise can also take pressure off your joints. After lifestyle factors, medicine can help relieve your arthritis pain. If over-the-counter medicines like acetaminophen, ibuprofen, or aspirin are not enough, your doctor may prescribe stronger medicines. Most forms of arthritis are long-term, and life-long, conditions. But if you make lifestyle changes, and work with your health care team to manage your pain, you should be able to move more freely and hopefully feel less pain.
Osteoarthritis - Animation
Osteoarthritis is the most common form of arthritis and is associated with the aging process. Even from the outside, you can see that the knee of an older person looks considerably different than that of a younger person. Let's take a look at the joint itself to see the differences. Osteoarthritis is a chronic disease, a disease that persists for a long time. It causes the deterioration of the cartilage within a joint. For most people, the cause of osteoarthritis is unknown, but metabolic, genetic, chemical, and mechanical factors play a role in its development. Symptoms of osteoarthritis include loss of flexibility, limited movement, and pain and swelling within the joint. The condition results from injury to the cartilage, which normally absorbs stress and covers the bones, so they can move smoothly. The cartilage of the affected joint is roughened and becomes worn down. As the disease progresses, the cartilage becomes completely worn down and the bone rubs on bone. Bony spurs usually develop around the margins of the joint. Part of the pain results from these bone spurs, which can restrict the joint's movement as well.
Rheumatoid arthritis - Animation
Most of us expect to become a little achy and creaky as we get older. It's because the cushion that protects our joints wears down over the years, a condition called osteoarthritis. But some people develop a form of arthritis at an earlier age, not because their joints are wearing away, but because their body is attacking and damaging their own joints. Let's talk about rheumatoid arthritis, or RA. The immune system normally keeps the body safe against bacteria, viruses, and other harmful invaders. But sometimes this system goes a little haywire, and the body mistakenly attacks its own tissues. That's known as an autoimmune disease. In the case of rheumatoid arthritis, the immune system attacks and damages your own joints. Like other forms of arthritis, rheumatoid arthritis makes the joints painful and stiff. If you have RA, you may notice that your joints feel stiffer in the morning, making it hard to get out of bed. Over time, you'll have trouble moving the affected joints, which can become deformed and bent out of shape. So, how do doctors diagnose rheumatoid arthritis?Well, there isn't one test that can tell for sure that you have RA. However, there are a couple of lab tests that can point your doctor to the diagnosis. You may also have an ultrasound, MRI, or x-rays so your doctor can see what's going on inside the affected joints. If you do have RA, many drugs can treat it. However, each of these drugs can have some side effects, and some of them are serious. You'll have to decide with your doctor which drug to take by weighing the benefits against the risks. If you're like most people with RA, you'll start by taking medicines called disease modifying antirheumatic drugs, or DMARDs for short. These include methotrexate. Often antimalarial drugs are given along with DMARDs. Anti-inflammatory medicines such as ibuprofen, naproxen, and celecoxib can help bring down the swelling in your joints. So can steroid drugs. If these medicines don't work, your doctor may suggest trying a biologic medicine, which targets the overactive immune response that's damaging your joints. Biologics are usually injected under the skin or into a vein. Severely deformed joints may need to be treated with surgery to remove the joint lining or even totally replace the damaged joint. Whatever treatment you use, also remember to exercise your joints on your own, or by going to a physical therapist. The right exercise can help keep your muscles strong and improve your joint mobility. When you have RA, don't try to overdo it. Think about your achy joints before doing any activity, so you don't overstress them. Also follow your doctor's treatment advice carefully. If you let this disease go, you could end up with permanent joint damage that can't be reversed. By treating RA early, you can get your joints, and the rest of you, moving more smoothly again.