Heart failure
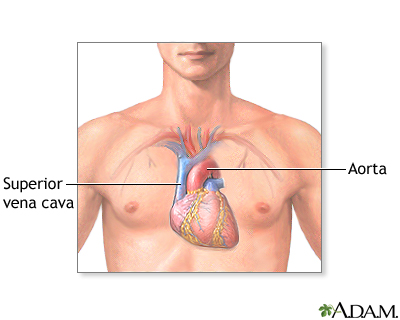
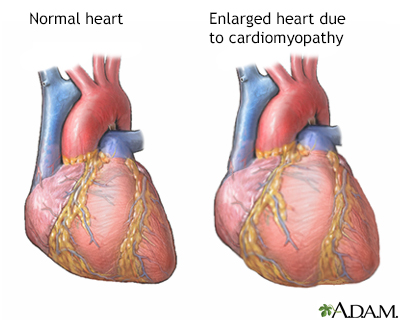
CHF; Congestive heart failure; Left-sided heart failure; Right-sided heart failure - cor pulmonale; Cardiomyopathy - heart failure; HFHeart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body.
The Basics
Tests for Congestive heart failure
A Closer Look
Primary pulmonary hypertension
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
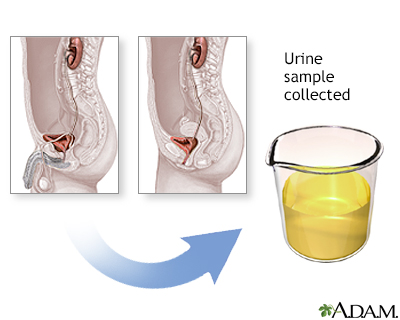
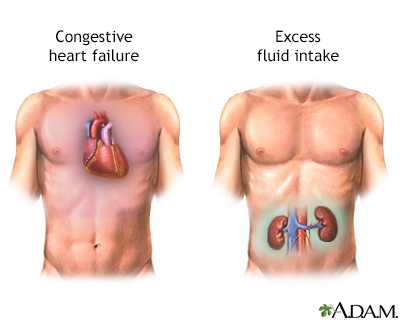
Osmolality test
An osmolality urine test is performed to measure the concentration of particles in urine. Greater than normal results may indicate conditions such as Addison disease, congestive heart failure or shock. Lower-than-normal measurements may indicate aldosteronism, diabetes insipidus, excess fluid intake, renal tubular necrosis or severe pyelonephritis.
Osmolality test
illustration
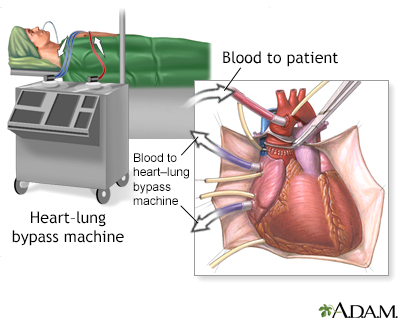
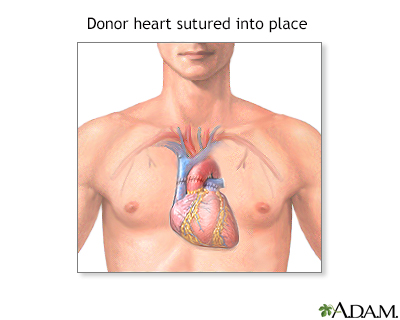
Heart transplant - series
Presentation
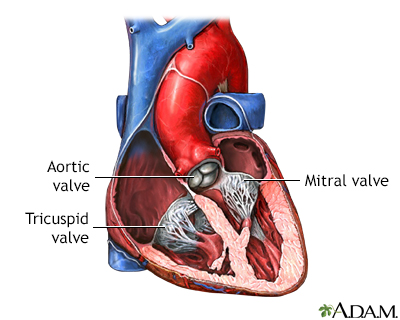
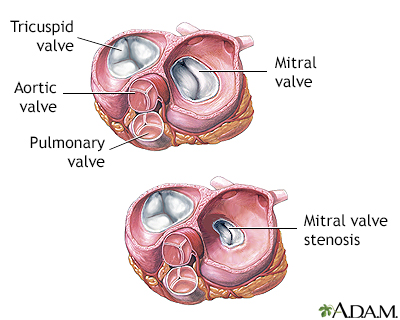
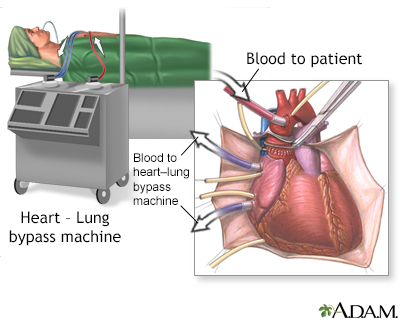
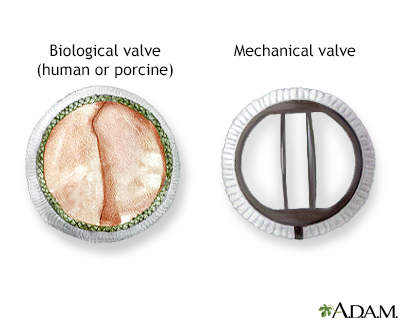
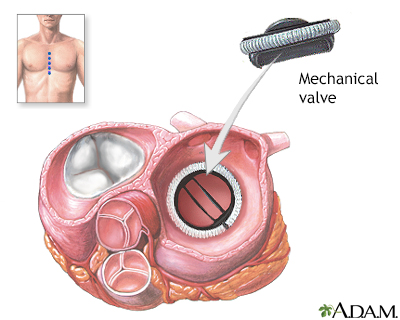
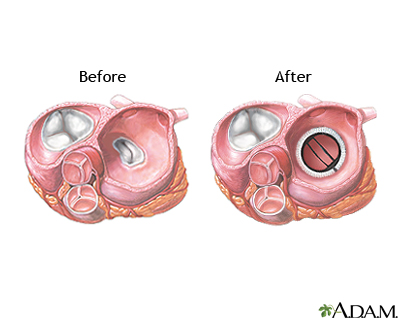
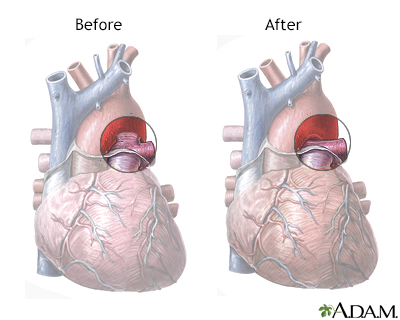
Heart valve surgery - series
Presentation
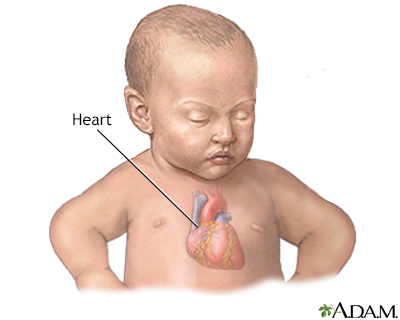
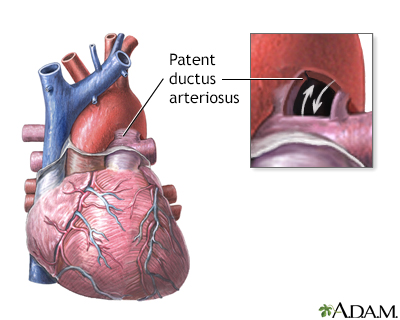
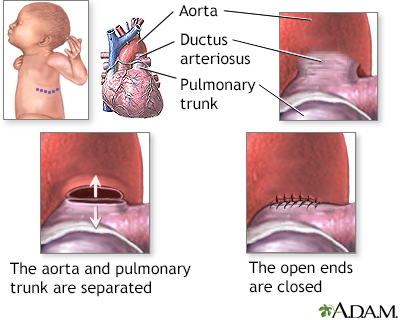
Patent ductus arteriosis (PDA) - series
Presentation
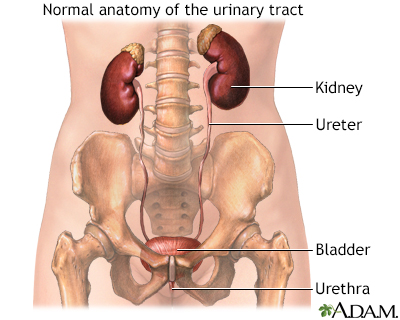
Osmolality urine - series
Presentation
Primary pulmonary hypertension
Pulmonary hypertension is the narrowing of the pulmonary arterioles within the lung. The narrowing of the arteries creates resistance and an increased work load for the heart. The heart becomes enlarged from pumping blood against the resistance. Some symptoms include chest pain, weakness, shortness of breath, and fatigue. The goal of treatment is control of the symptoms, although the disease usually develops into congestive heart failure.
Primary pulmonary hypertension
illustration
Osmolality test
An osmolality urine test is performed to measure the concentration of particles in urine. Greater than normal results may indicate conditions such as Addison disease, congestive heart failure or shock. Lower-than-normal measurements may indicate aldosteronism, diabetes insipidus, excess fluid intake, renal tubular necrosis or severe pyelonephritis.
Osmolality test
illustration
Heart transplant - series
Presentation
Heart valve surgery - series
Presentation
Patent ductus arteriosis (PDA) - series
Presentation
Osmolality urine - series
Presentation
Heart failure
CHF; Congestive heart failure; Left-sided heart failure; Right-sided heart failure - cor pulmonale; Cardiomyopathy - heart failure; HFHeart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body.
The Basics
Tests for Congestive heart failure
A Closer Look
Heart failure
CHF; Congestive heart failure; Left-sided heart failure; Right-sided heart failure - cor pulmonale; Cardiomyopathy - heart failure; HFHeart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body.
The Basics
Tests for Congestive heart failure
A Closer Look
Review Date: 7/14/2024
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.