Gastroesophageal reflux disease
Peptic esophagitis; Reflux esophagitis; GERD; Heartburn - chronic; DyspepsiaGastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). Food travels from your mouth to the stomach through your esophagus. GERD can irritate the food pipe and cause heartburn and other symptoms.
The Basics
Tests for gastroesophageal reflux disease
A Closer Look
Self Care
Talking to your MD
Gastroesophageal reflux disease - Animation
Gastroesophageal reflux disease
Animation
Anti-reflux surgery - Animation
Anti-reflux surgery
Animation
Gastroesophageal reflux disease
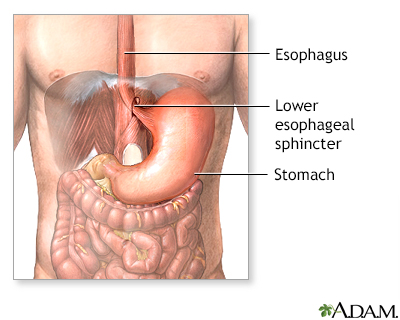
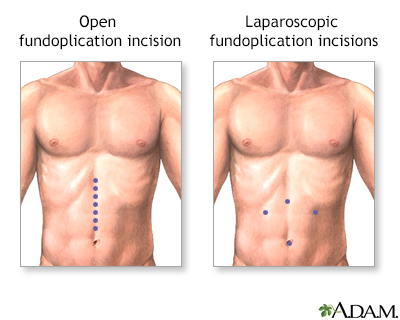
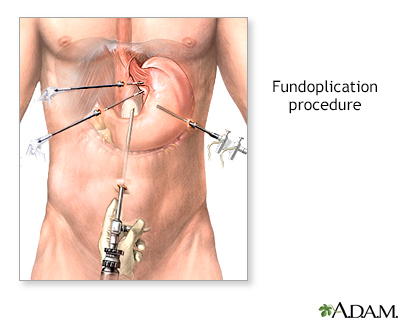
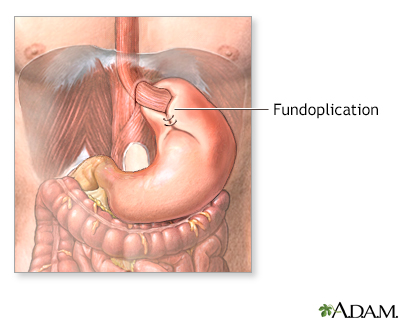
A band of muscle fibers, the lower esophageal sphincter, closes off the esophagus from the stomach. If the sphincter does not close properly, food and liquid can move backward into the esophagus and cause heartburn and other symptoms known as gastroesophageal disease (GERD). To alleviate symptoms, dietary changes and medications are prescribed. For a patient who has persistent symptoms despite medical treatment, an anti-reflux operation may be an option.
Gastroesophageal reflux disease
illustration
Heartburn prevention
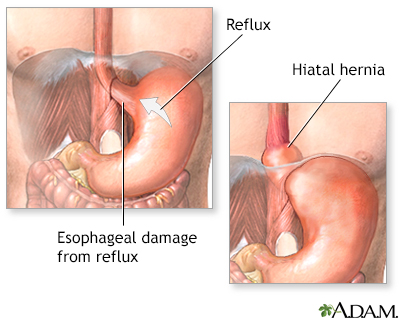
Heartburn is a condition where the acidic stomach contents back up into the esophagus causing pain in the chest area. This reflux usually occurs because the sphincter muscle between the esophagus and stomach is weakened. Standing or sitting after a meal can help reduce the reflux which causes heartburn. Continuous irritation of the esophagus lining as in gastroesophageal reflux disease is a risk factor for the development of adenocarcinoma.
Heartburn prevention
illustration
Gastroesophageal reflux - series
Presentation
Gastroesophageal reflux disease - Animation
Gastroesophageal reflux disease
Animation
Anti-reflux surgery - Animation
Anti-reflux surgery
Animation
Gastroesophageal reflux disease
A band of muscle fibers, the lower esophageal sphincter, closes off the esophagus from the stomach. If the sphincter does not close properly, food and liquid can move backward into the esophagus and cause heartburn and other symptoms known as gastroesophageal disease (GERD). To alleviate symptoms, dietary changes and medications are prescribed. For a patient who has persistent symptoms despite medical treatment, an anti-reflux operation may be an option.
Gastroesophageal reflux disease
illustration
Heartburn prevention
Heartburn is a condition where the acidic stomach contents back up into the esophagus causing pain in the chest area. This reflux usually occurs because the sphincter muscle between the esophagus and stomach is weakened. Standing or sitting after a meal can help reduce the reflux which causes heartburn. Continuous irritation of the esophagus lining as in gastroesophageal reflux disease is a risk factor for the development of adenocarcinoma.
Heartburn prevention
illustration
Gastroesophageal reflux - series
Presentation
Gastroesophageal reflux disease
Peptic esophagitis; Reflux esophagitis; GERD; Heartburn - chronic; DyspepsiaGastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). Food travels from your mouth to the stomach through your esophagus. GERD can irritate the food pipe and cause heartburn and other symptoms.
The Basics
Tests for gastroesophageal reflux disease
A Closer Look
Self Care
Talking to your MD
Gastroesophageal reflux disease
Peptic esophagitis; Reflux esophagitis; GERD; Heartburn - chronic; DyspepsiaGastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). Food travels from your mouth to the stomach through your esophagus. GERD can irritate the food pipe and cause heartburn and other symptoms.
The Basics
Tests for gastroesophageal reflux disease
A Closer Look
Self Care
Talking to your MD
Review Date: 1/24/2025
Reviewed By: Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.