Unstable angina
Accelerating angina; New-onset angina; Angina - unstable; Progressive angina; CAD - unstable angina; Coronary artery disease - unstable angina; Heart disease - unstable angina; Chest pain - unstable anginaUnstable angina is a condition in which your heart doesn't get enough blood flow and oxygen. It may lead to a heart attack.
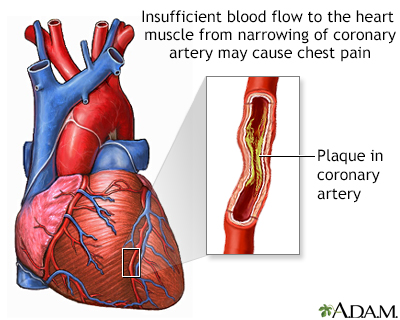
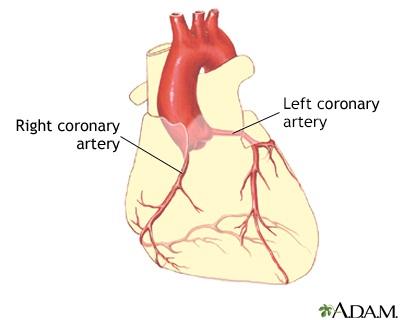
Angina is a type of chest discomfort due to poor blood flow through the blood vessels in the heart called the coronary arteries.
-
Causes
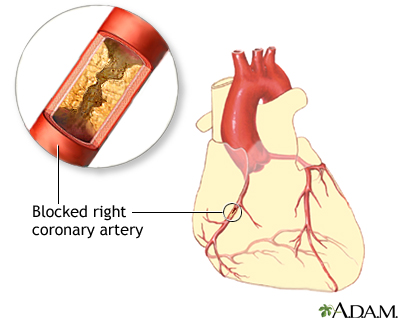
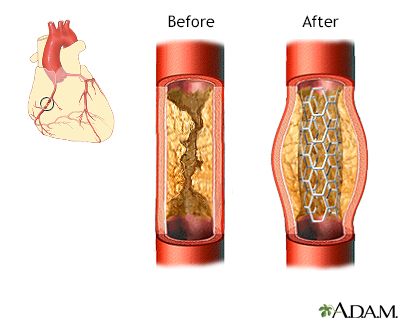
Coronary artery disease due to atherosclerosis is the most common cause of unstable angina. Atherosclerosis is the buildup of fatty material, called plaque, along the walls of the arteries. This causes arteries to become narrowed and less flexible. The narrowing can reduce blood flow to the heart, causing chest pain.
People with unstable angina are at higher risk of having a heart attack.
Less common causes of angina are:
- Abnormal function of tiny branch arteries without narrowing of larger arteries (called microvascular dysfunction or Syndrome X)
- Coronary artery spasm
Risk factors for coronary artery disease include:
- Diabetes
- Family history of early coronary heart disease (a close relative such as a sibling or parent had heart disease before age 55 in a man or before age 65 in a woman)
- High blood pressure
- High LDL cholesterol
- Low HDL cholesterol
- Male sex
- Sedentary lifestyle (not getting enough exercise)
- Obesity
- Older age
- Smoking
-
Symptoms
Symptoms of angina may include:
- Chest pain that you may also feel in the shoulder, arm, jaw, neck, back, or other area
- Discomfort that feels like tightness, squeezing, crushing, burning, choking, or aching
- Discomfort that occurs at rest and does not easily go away when you take medicine
- Shortness of breath
- Sweating
With stable angina, the chest pain or other symptoms only occur with a certain amount of activity or stress. The pain does not occur more often or get worse over time.
Unstable angina is chest pain that is sudden and often gets worse over a short period of time. You may be developing unstable angina if your chest pain:
- Starts to feel different, is more severe, comes more often, or occurs with less activity or while you are at rest
- Lasts longer than 15 to 20 minutes
- Occurs without cause (for example, while you are asleep or sitting quietly)
- Does not respond well to a medicine called nitroglycerin (especially if this medicine worked to relieve chest pain in the past)
- Occurs with a drop in blood pressure or shortness of breath
Unstable angina is a warning sign that a heart attack may happen soon and needs to be treated right away. Contact your health care provider if you have any type of chest pain.
-
Exams and Tests
Your provider will do a physical exam and check your blood pressure. Your provider may hear abnormal sounds, such as a heart murmur or irregular heartbeat, when listening to your chest with a stethoscope.
Tests for angina include:
- Blood tests to show if you have heart tissue damage or are at a high risk for heart attack, including high sensitivity cardiac troponins I and T. Testing may also include creatine phosphokinase (CPK), and myoglobin.
- Electrocardiogram (ECG).
- Echocardiography.
- Stress tests, such as exercise tolerance test (stress test or treadmill test), nuclear stress test, or stress echocardiogram.
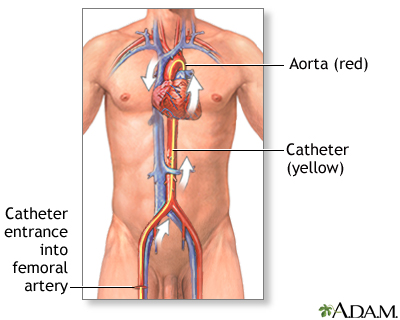
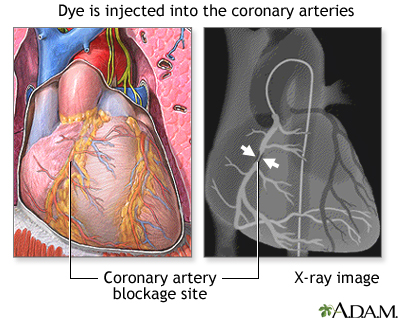
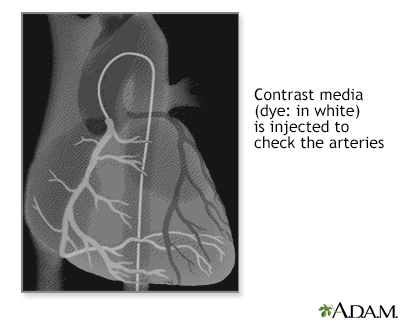
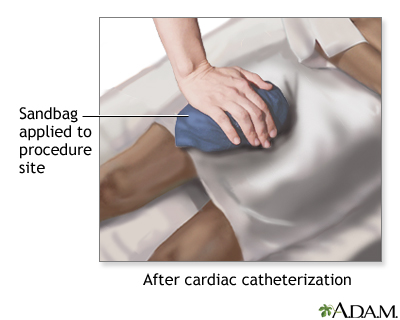
- Coronary angiography. This test involves taking pictures of the heart arteries using x-rays and dye. It is the most direct test to diagnose heart artery narrowing and find clots.
-
Treatment
You may need to check into the hospital to get some rest, have more tests, and prevent complications.
Blood thinners (antiplatelet medicines) are used to treat and prevent unstable angina. You will receive these drugs as soon as possible if you can take them safely. Medicines include aspirin and the prescription medicine clopidogrel or something similar (ticagrelor, prasugrel). These medicines may be able to reduce the chance of a heart attack or the severity of a heart attack that occurs.
During an unstable angina event:
- You may get heparin (or another blood thinner) and nitroglycerin (under your tongue or through an IV).
- Other treatments may include medicines to control blood pressure, anxiety, abnormal heart rhythms, and cholesterol (such as a statin drug).
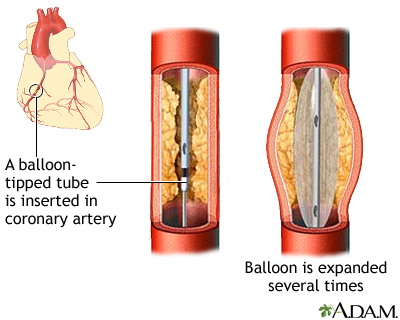
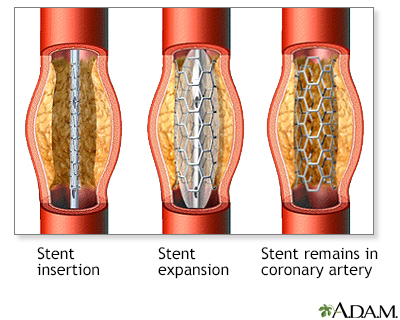
A procedure called angioplasty and stenting can often be done to open a blocked or narrowed artery.
- Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to the heart.
- A coronary artery stent is a small, metal mesh tube that opens up (expands) inside a coronary artery. A stent is often placed after angioplasty. It helps prevent the artery from closing up again. A drug-eluting stent has medicine in it that helps prevent the artery from closing over time.
Heart bypass surgery may be done for some people. The decision to have this surgery depends on:
- Which arteries are blocked
- How many arteries are involved
- Which parts of the coronary arteries are narrowed
- How severe the narrowings are
-
Outlook (Prognosis)
Unstable angina is a sign of more severe heart disease.
How well you do depends on many different things, including:
- How many and which arteries in your heart are blocked, and how severe the blockage is
- If you have ever had a heart attack
- How well your heart muscle is able to pump blood out to your body
Abnormal heart rhythms and heart attacks can cause sudden death.
-
Possible Complications
Unstable angina may lead to:
- Abnormal heart rhythms (arrhythmias)
- A heart attack
- Heart failure
-
When to Contact a Medical Professional
Seek medical attention right away if you have new, unexplained chest pain or pressure. If you have had angina before, contact your provider.
Call 911 or the local emergency number if your angina pain:
- Is not better 5 minutes after you take nitroglycerin (your provider may tell you to take 3 total doses)
- Does not go away after 3 doses of nitroglycerin
- Is getting worse
- Returns after the nitroglycerin helped at first
Contact your provider if:
- You are having angina symptoms more often
- You are having angina when you are sitting (rest angina)
- You are feeling tired more often
- You are feeling faint or lightheaded, or you pass out
- Your heart is beating very slowly (less than 60 beats a minute) or very fast (more than 120 beats a minute), or it is not steady
- You are having trouble taking your heart medicines
- You have any other unusual symptoms
If you think you are having a heart attack, get medical treatment right away.
-
Prevention
Some studies have shown that making a few lifestyle changes can prevent blockages from getting worse and may actually improve them. Lifestyle changes can also help prevent some angina attacks. Your provider may tell you to:
- Lose weight if you are overweight
- Stop smoking
- Exercise regularly
- Drink alcohol in moderation only
- Eat a healthy diet that is high in vegetables, fruits, whole grains, fish, and lean meats
Your provider will also recommend that you keep other health conditions such as high blood pressure, diabetes, and high cholesterol levels under control.
If you have one or more risk factors for heart disease, talk to your provider about taking aspirin or other medicines to help prevent a heart attack. Aspirin therapy (75 to 325 mg a day) or medicines such as clopidogrel, ticagrelor or prasugrel may help prevent heart attacks in some people. Aspirin and other blood-thinning therapies are recommended if the benefit is likely to outweigh the risk of side effects.
References
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. [Published correction appears in J Am Coll Cardiol. 2014;64(24):2713-2714. Dosage error in article text]. J Am Coll Cardiol. 2014;64(24):e139-e228. PMID: 25260718 pubmed.ncbi.nlm.nih.gov/25260718/.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. [published correction appears in Circulation. 2019;140(11):e649-e650] [published correction appears in Circulation. 2020;141(4):e60] [published correction appears in Circulation. 2020;141(16):e774]. Circulation. 2019;140(11):e596-e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 39.
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454. PMID: 34709879 pubmed.ncbi.nlm.nih.gov/34709879/.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the Management of Acute Myocardial Infarction in Patients Presenting with ST-segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. PMID: 28886621 pubmed.ncbi.nlm.nih.gov/28886621/.
Lange RA, Mukherjee D. Acute coronary syndrome: unstable angina and non-ST elevation myocardial infarction. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 57.
Writing Committee Members, Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187-e285. PMID: 34756653 pubmed.ncbi.nlm.nih.gov/34756653/.