Breast cancer
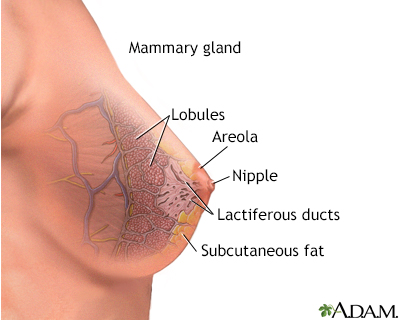
Cancer - breast; Carcinoma - ductal; Carcinoma - lobular; DCIS; LCIS; HER2-positive breast cancer; ER-positive breast cancer; Ductal carcinoma in situ; Lobular carcinoma in situBreast cancer is cancer that starts in the tissues of the breast. There are two main types of breast cancer:
- Ductal carcinoma starts in the tubes (ducts) that carry milk from the breast to the nipple. Most breast cancers are of this type.
- Lobular carcinoma starts in the parts of the breast, called lobules, which produce milk.
In rare cases, other kinds of breast cancer can start in other areas of the breast.
-
Causes
Breast cancer risk factors are things that increase the chance that you could develop breast cancer:
- Some risk factors you can control, such as drinking alcohol. Others, such as age and family history, you cannot control.
- The more risk factors you have, the more your risk increases. But, it does not mean you will develop cancer. Most women who develop breast cancer do not have known risk factors or a family history.
- Understanding your risk factors can help you take steps to lower your risk.
Some women are at higher risk for breast cancer because of certain genetic changes or variants that may be passed down from their parents.
- Genes known as BRCA1 or BRCA2 are responsible for most cases of inherited breast cancers.
- A screening tool with questions about your and your family's medical history can help your health care provider determine whether you are at risk for carrying these genes.
- If you may be at high risk due to a known variant gene such as BRCA1 or BRCA2, a blood test can show if you carry the genes.
- Certain other genes may lead to an increased risk of breast cancer.
Breast implants, using antiperspirants, and wearing underwire bras do not increase the risk for breast cancer. There is also no evidence of a direct link between breast cancer and pesticides.
-
Symptoms
Early breast cancer often does not cause symptoms. This is why regular breast cancer screening is important, so cancers that don't have symptoms may be found earlier.
As the cancer grows, symptoms may include:
- Breast lump or lump in the armpit that is hard, has uneven edges, and usually does not hurt.
- Change in the size, shape, or feel of the breast or nipple. For example, you may have redness, dimpling, or puckering that looks like the skin of an orange.
- Fluid from the nipple. Fluid may be bloody, clear to yellow, green, or look like pus.
In men, breast cancer symptoms include breast lump, breast pain, and breast tenderness.
Symptoms of advanced breast cancer may include:
- Bone pain
- Shortness of breath
- Swelling of the lymph nodes in the armpit (next to the breast with cancer)
- Weight loss
-
Exams and Tests
Your provider will ask about your symptoms and risk factors. Then they will perform a physical exam. The exam includes both breasts, armpits, and the neck and chest area.
Women may choose to perform breast self-exams each month. However, the effectiveness of self-exams for detecting breast cancer is debatable.
Tests used to diagnose and monitor people with a breast lump or breast cancer may include:
- Mammography to screen for breast cancer or help identify a breast lump
- Breast ultrasound to show whether a lump is solid or fluid-filled
- Breast MRI to help better identify a breast lump or evaluate an abnormal change on a mammogram
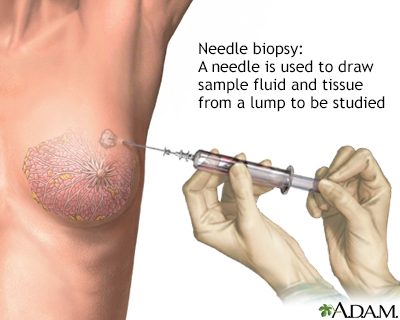
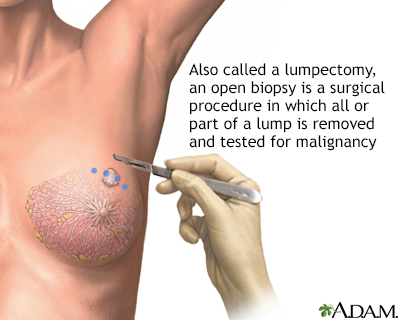
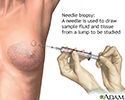
- Breast biopsy, using methods such as needle aspiration or ultrasound-guided, stereotactic, or open biopsy
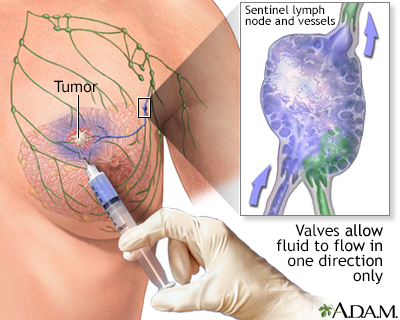
- Sentinel lymph node biopsy to check if the cancer has spread to the lymph nodes
- CT scan to check if the cancer has spread outside the breast
- PET scan to check if the cancer has spread outside the breast
If your provider learns that you do have breast cancer, more tests will be done. This is called staging, which checks if the cancer has spread. Staging helps guide treatment and follow-up. It also gives you an idea of what to expect in the future.
Breast cancer stages range from 0 to IV. The higher the stage, the more advanced the cancer.
-
Treatment
Treatment is based on many factors, including:
- The type of breast cancer
- The stage of the cancer (staging is a tool your providers use to find out how advanced the cancer is)
- Whether the cancer is sensitive to certain hormones, mainly estrogen and progesterone
- Whether the cancer overproduces (overexpresses) the HER2/neu protein
- Tests on the tumor's genes to see if you would benefit from chemotherapy
Cancer treatments may include:
- Hormone therapy.
- Chemotherapy, which uses medicines to kill cancer cells.
- Radiation therapy, which is used to destroy cancerous tissue.
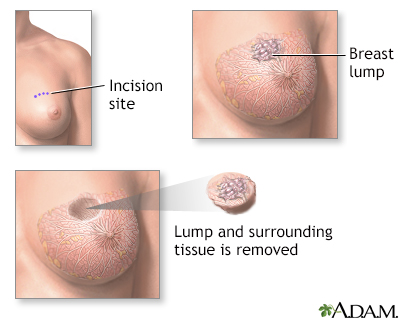
- Surgery to remove cancerous tissue: A lumpectomy removes the breast lump. A mastectomy removes all or part of the breast and possibly nearby structures. Nearby lymph nodes may also be removed during surgery.
- Targeted therapy which uses medicine to attack the gene changes in cancer cells. Hormone therapy is an example of targeted therapy. It blocks certain hormones that fuel cancer growth. Other targeted therapy medicines are not related to hormones.
Cancer treatment can be local or systemic:
- Local treatments involve only the area of disease. Radiation and surgery are forms of local treatment. They are most effective when the cancer has not spread outside the breast.
- Systemic treatments affect the entire body. Chemotherapy and hormonal therapy are types of systemic treatment.
Most women receive a combination of treatments. For women with stage I, II, or III breast cancer, the main goal is to treat the cancer and prevent it from returning (recurring). For women with stage IV cancer, the goal is to improve symptoms and help them live longer. In most cases, stage IV breast cancer cannot be cured.
- Stage 0 (for example, ductal carcinoma in-situ) and ductal carcinoma: Lumpectomy plus radiation or mastectomy is the standard treatment.
- Stage I and II: Lumpectomy plus radiation or mastectomy with lymph node removal is the standard treatment. Chemotherapy, hormonal therapy, and other targeted therapy may also be used after surgery.
- Stage III: Treatment involves surgery, possibly preceded or followed by chemotherapy, hormone therapy, and other targeted therapy.
- Stage IV: Treatment may involve surgery, radiation, chemotherapy, hormone therapy, other targeted therapy, or a combination of these treatments.
After treatment, some women continue to take medicines for some time, often several years. All women continue to have mammograms to monitor for the return of cancer or development of another breast cancer.
Women who have had a mastectomy may have reconstructive breast surgery. This will be done either at the time of mastectomy or later.
-
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
-
Outlook (Prognosis)
New, improved treatments are helping people with breast cancer live longer. Even with treatment, breast cancer can spread to other parts of the body. Sometimes, breast cancer returns, even after the entire tumor has been removed and nearby lymph nodes are found to be cancer-free.
Some women who have had breast cancer develop a new breast cancer that is not related to the original tumor.
How well you do after being treated for breast cancer depends on many things. The more advanced your cancer, the worse the outcome. Other factors that determine the risk for recurrence and the likelihood of successful treatment include:
- Location of the tumor and how far it has spread
- Whether the tumor is hormone receptor-positive or -negative
- Gene expression
- Tumor size and shape
After considering all of the above, your provider can discuss your risk of having a recurrence of breast cancer.
-
Possible Complications
You may experience side effects or complications from cancer treatment. These may include temporary pain or swelling of the breast and surrounding area. Ask your provider about the possible side effects from treatment.
-
When to Contact a Medical Professional
Contact your provider if:
- You have a breast or armpit lump
- You have nipple discharge
After being treated for breast cancer, contact your provider if you develop symptoms such as:
- Nipple discharge
- Rash on the breast
- New lumps in the breast
- Swelling in the area
- Pain, especially chest pain, abdominal pain, or bone pain
-
Prevention
Talk to your provider about how often you should have a mammogram or other tests to screen for breast cancer. Early breast cancers found by a mammogram have a good chance of being cured.
Mammography is performed to screen women to detect early breast cancer when it is more likely to be cured. The recommendations of different expert organizations can differ.
- Mammography is generally recommended for all women starting at age 40, repeated every 1 to 2 years.
- Women with a family history of breast cancer should work with their provider to assess their risk of breast cancer. In some situations, additional testing may be considered.
Mammograms work best at finding breast cancer in women ages 40 to 74. It is not clear how well mammograms work at finding cancer in women age 75 and older.
Tamoxifen is approved for breast cancer prevention in women age 35 and older who are at high risk. Raloxifene is approved for breast cancer prevention in women after the menopause. Discuss this with your provider.
Women at very high risk for breast cancer may consider preventive (prophylactic) mastectomy. This is surgery to remove the breasts before breast cancer is diagnosed. Possible candidates include:
- Women who have already had one breast removed due to cancer
- Women with a strong family history of breast cancer
- Women with genes or genetic mutations that raise their risk for breast cancer (such as BRCA1 or BRCA2)
Many risk factors, such as your genes and family history, cannot be controlled. But making healthy lifestyle changes may reduce your overall chance of getting cancer. This includes:
- Eating healthy foods
- Maintaining a healthy weight
- Limiting alcohol consumption to 1 drink per day
References
Harnden K, Mauro L, Pennisi A. Breast cancer. In: Ginsburg GS, Willard HF, Strickler JH, McKinney MS, eds. Genomic and Precision Medicine: Oncology. 3rd ed. Philadelphia, PA: Elsevier; 2022:chap 9.
Korourian S, Klimberg VS. Clinical prognosis and staging of breast cancer. In: Klimberg VS, Gradishar WJ, Bland KI, et al, eds. Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Philadelphia, PA: Elsevier; 2024:chap 26.
National Cancer Institute website. Breast cancer treatment (PDQ) - health professional version. www.cancer.gov/types/breast/hp/breast-treatment-pdq. Updated March 14, 2025. Accessed April 22, 2025.
National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN guidelines): Breast cancer. Version 1.2025. www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Updated January 31, 2025. Accessed February 11, 2025.
US Preventive Services Task Force, Nicholson WK, Silverstein M, et al. Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2024;331(22):1918-1930. PMID: 38687503 pubmed.ncbi.nlm.nih.gov/38687503/.
US Preventive Services Task Force, Owens DK, Davidson KW, et al. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322(7):652-665. PMID: 31429903 pubmed.ncbi.nlm.nih.gov/31429903/.