Cervical cancer
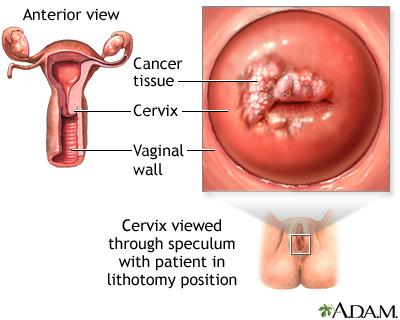
Cancer - cervix; Cervical cancer - HPV; Cervical cancer - dysplasiaCervical cancer is cancer that starts in the cervix. The cervix is the lower part of the uterus (womb) that opens at the top of the vagina.
-
Causes
Worldwide, cervical cancer is the fourth most common type of cancer in women. It is much less common in the United States because of the widespread use of Pap tests to screen women for cervical cancer or its precursors.
Cervical cancer starts in the cells on the surface of the cervix. There are two types of cells on the surface of the cervix, squamous and columnar (gland cells). Most cervical cancers are from squamous cells.
Cervical cancer usually develops slowly. It starts as a precancerous condition called dysplasia. This condition can be detected by a Pap test and is nearly 100% treatable. It can take years for dysplasia to develop into cervical cancer. Most women who are diagnosed with cervical cancer today have not had regular Pap tests or the HPV vaccine, or they have not followed up on abnormal Pap test results.
Almost all cervical cancers are caused by human papillomavirus (HPV). HPV is a common virus that is spread through skin-to-skin contact and also by sexual intercourse. There are many different types (strains) of HPV. Some strains lead to cervical as well as other cancers. Other strains can cause genital warts. Others do not cause any problems at all.
A woman's sexual behavior can increase her risk for developing cervical cancer. Risky sexual practices include:
- Having sex at an early age
- Having multiple sexual partners
- Having a partner or many partners who take part in high-risk sexual activities
Other risk factors for cervical cancer include:
- Not getting the HPV vaccine
- Being economically disadvantaged
- Having a mother who took the medicine diethylstilbestrol (DES) during pregnancy in the early 1960s to prevent miscarriage
- Having a weakened immune system
-
Symptoms
Most of the time, early cervical cancer has no symptoms. Symptoms that may occur include:
- Abnormal vaginal bleeding between periods, after intercourse, or after menopause
- Vaginal discharge that does not stop, and may be pale, watery, pink, brown, bloody, or foul-smelling
- Periods that become heavier and last longer than usual
Cervical cancer may spread to the vagina, lymph nodes, bladder, intestines, lungs, bones, and liver. Often, there are no problems or symptoms until the cancer is advanced and has spread. Symptoms of advanced cervical cancer may include:
- Abdominal pain
- Back pain
- Bone pain or fractures
- Fatigue
- Leaking of urine or feces from the vagina
- Leg pain
- Loss of appetite
- Pelvic pain
- Single swollen leg
- Weight loss
-
Exams and Tests
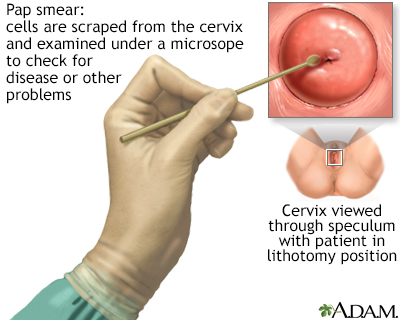
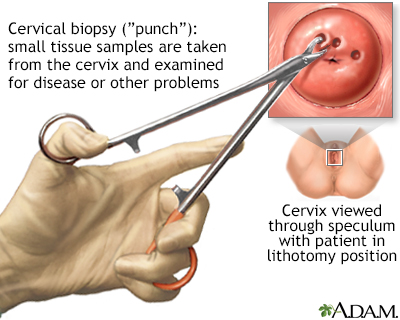
Precancerous changes of the cervix and cervical cancer cannot be seen with the naked eye. Special tests and tools are needed to spot such conditions:
- A Pap test screens for precancers and cancer, but does not make a final diagnosis.
- Depending on your age, the HPV DNA test may be done along with a Pap test to screen for cervical cancer. Or it may be used after a woman has had an abnormal Pap test result. It may also be used as the first test. Talk to your health care provider about which test or tests are right for you.
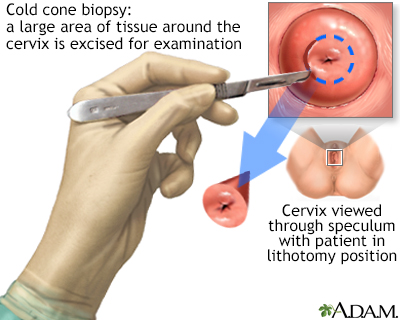
- If abnormal changes are found, the cervix is usually examined under magnification. This procedure is called colposcopy. Pieces of tissue might be removed (biopsied) during this procedure. This tissue is then sent to a lab for examination.
- A procedure called a loop electrosurgical excision procedure (LEEP) may also be done. This uses an electrified metal loop to remove some tissue from the cervix. If this is not feasible, a larger procedure called a cone biopsy may be done. This is a procedure that removes a cone-shaped wedge from the front of the cervix.
If cervical cancer is diagnosed, the provider will order more tests. These help determine how far the cancer has spread. This is called cancer staging. Tests may include:
-
Treatment
Treatment of cervical cancer depends on:
- The stage of the cancer
- The size and shape of the tumor
- The woman's age and general health
- Her desire to have children in the future
Early cervical cancer can be cured by removing or destroying the precancerous or cancerous tissue. This is why Pap tests done at the recommended times are so important to prevent cervical cancer, or catch it at an early stage. There are surgical ways to cure cervical cancer without removing the uterus or seriously damaging the cervix, so that a woman can still have children in the future.
Types of surgery for cervical precancer, and on occasion, very small early cervical cancer include:
- LEEP -- uses electricity to remove abnormal tissue.
- Cold knife cone -- uses a scalpel to remove abnormal tissue.
- Cryotherapy -- freezes abnormal cells.
- Laser therapy -- uses light to burn abnormal tissue.
- Hysterectomy may be done for women with precancer who have undergone multiple LEEP procedures, or who are not interested in further childbearing.
Treatment for more advanced cervical cancer may include:
- Radical hysterectomy, which removes the uterus and much of the surrounding tissues, including lymph nodes and the upper part of the vagina. This is more often performed on younger, healthier women with small tumors.
- Radiation therapy, along with low dose chemotherapy, is more often used for women with tumors too large for radical hysterectomy or women who are not good candidates for surgery.
- Pelvic exenteration, an extreme type of surgery in which all of the organs of the pelvis, including the bladder and rectum, are removed.
Radiation therapy may also be used to treat cancer that has returned.
Chemotherapy uses medicines to kill cancer. It may be given alone or with surgery or radiation.
-
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
-
Outlook (Prognosis)
How well the person does depends on many things, including:
- The type of cervical cancer
- The stage of cancer (how far it has spread)
- Age and general health
- If the cancer comes back after treatment
Precancerous conditions can be completely cured when followed up and treated properly. Most women are alive in 5 years (5-year survival rate) for cancer that has spread to the inside of the cervix walls but not outside the cervix area. The 5-year survival rate falls as the cancer spreads outside the walls of the cervix into other areas.
-
Possible Complications
Complications can include:
- Risk of the cancer coming back especially in women who have treatment to save the uterus
- Problems with sexual, bowel, and bladder function after surgery or radiation
-
When to Contact a Medical Professional
Contact your provider if you:
- Have not had regular Pap tests
- Have abnormal vaginal bleeding or discharge
-
Prevention
Cervical cancer can be prevented by doing the following:
- Get the HPV vaccine. The vaccine prevents most types of HPV infection that cause cervical cancer. Your provider can tell you if the vaccine is right for you.
- Practice safer sex. Using condoms during sex reduces the risk for HPV and other sexually transmitted infections (STIs).
- Limit the number of sexual partners you have. Avoid partners who are active in high-risk sexual behaviors.
- Get Pap tests as often as your provider recommends. Pap tests can help detect early changes, which can be treated before they turn into cervical cancer.
- Get the HPV test if recommended by your provider. It can be used along with the Pap test to screen for cervical cancer in women 30 years and older, or for some screening protocols, starting at age 25.
- If you smoke, quit. Smoking increases your chance of getting cervical cancer.
References
Centers for Disease Control and Prevention website. Clinical overview of HPV. www.cdc.gov/hpv/hcp/clinical-overview/index.html. Updated July 9, 2024. Accessed January 17, 2025.
National Cancer Institute website. Cervical cancer treatment (PDQ) - health professional version. www.cancer.gov/types/cervical/hp/cervical-treatment-pdq. Updated July 23, 2024. Accessed January 17, 2025.
Salcedo MP, Phoolcharoen N, Schmeler KM. Intraepithelial neoplasia of the lower genital tract (cervix, vagina, vulva): etiology, screening, diagnosis, management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 29.
US Preventive Services Task Force website. Final recommendation statement. Cervical cancer: screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening. Last updated July 23, 2024. . Accessed January 17, 2025.