Achalasia
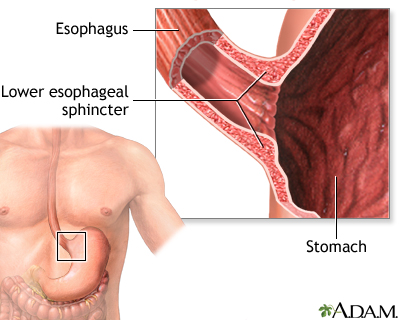
Esophageal achalasia; Swallowing problems for liquids and solids; Cardiospasm - lower esophageal sphincter spasmThe tube that carries food from the mouth to the stomach is the esophagus or food pipe. Achalasia makes it harder for the esophagus to move food into the stomach.
-
Causes
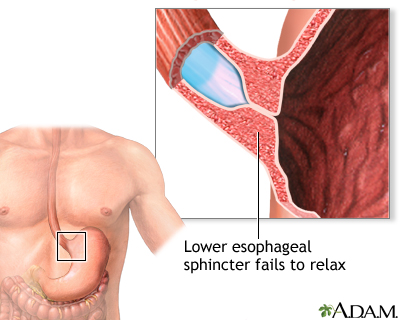
There is a muscular ring at the point where the esophagus and stomach meet. It is called the lower esophageal sphincter (LES). Normally, this muscle relaxes when you swallow to allow food to pass into the stomach. In people with achalasia, it does not relax as it should. In addition, the normal muscle activity of the esophagus (peristalsis) is reduced or absent.
This problem is caused by damage to the nerves of the esophagus.
Other problems can cause similar symptoms, such as cancer of the esophagus or upper stomach, and a parasite infection that causes Chagas disease, which is more common in Mexico and Central and South America.
Achalasia is rare. It may occur at any age, but is most common in people ages 25 to 60. In some people, the problem may be inherited.
-
Symptoms
Symptoms include:
- Backflow (regurgitation) of food
- Chest pain, which may increase after eating, or may be felt as pain in the back, neck, and arms
- Cough
- Difficulty swallowing liquids and solids
- Heartburn
- Unintentional weight loss
-
Exams and Tests
Physical exam may show signs of anemia or malnutrition.
Tests include:
- Esophageal manometry, a test to measure if your esophagus is working properly.
- Functional luminal imaging probe (FLIP). Creates a high resolution 3D image of your esophagus and its movements.
- EGD or upper endoscopy, a test to examine the lining of the stomach and esophagus. It uses a flexible tube and camera.
- Upper GI x-ray.
-
Treatment
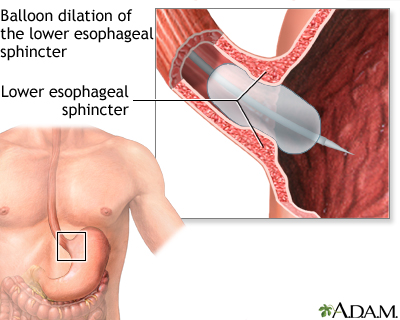
The goal of treatment is to reduce the pressure at the sphincter muscle and allow food and liquids to pass easily into the stomach. Therapy may involve:
- Injection with botulinum toxin (Botox) -- This may help relax the sphincter muscles. However, the benefit wears off within a few weeks or months.
- Medicines, such as long-acting nitrates or calcium channel blockers -- These medicines can be used to relax the lower esophagus sphincter. But there is rarely a long-term solution with medicines to treat achalasia.
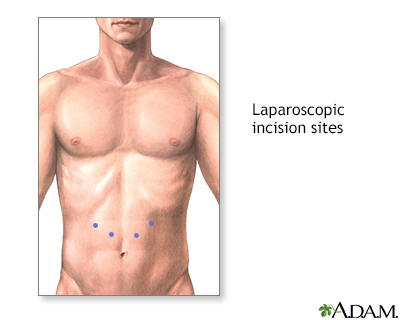
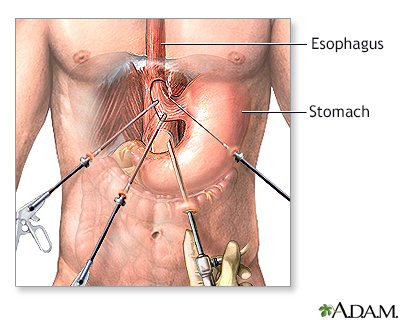
- Surgery (called a myotomy) -- In this procedure, the lower sphincter muscle is cut. This procedure is usually performed using a laparoscope. It can now sometimes be performed during EGD instead of traditional surgery.
- Widening (dilation) of the esophagus -- This is done during EGD by stretching the LES with a balloon dilator.
Your health care provider can help you decide which treatment is best for you.
-
Outlook (Prognosis)
The outcomes of surgery and non-surgical treatments are similar. However, depending on the type of achalasia you have, your provider may recommend a particular procedure. More than one treatment is sometimes necessary.
-
Possible Complications
Complications may include:
- Backflow (regurgitation) of acid or food from the stomach into the esophagus (reflux)
- Breathing food contents into the lungs (aspiration), which can cause pneumonia
- Tearing (perforation) of the esophagus
-
When to Contact a Medical Professional
Contact your provider if:
- You have trouble swallowing or painful swallowing
- Your symptoms continue, even with treatment for achalasia
-
Prevention
Many of the causes of achalasia cannot be prevented. However, treatment may help to prevent complications.
References
Bok-yan So J. The management of achalasia and other motility disorders of the oesophagus. In: Lamb PJ, ed. Oesophagogastric Surgery: A Companion to Specialist Surgical Practice. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 14.
Falk GW, Katzka DA. Diseases of the esophagus. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 124.
Pandolfino JE, Kahrilas PJ. Esophageal neuromuscular function and motility disorders. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 44.