Triglyceride level
Triacylglycerol testThe triglyceride level is a blood test to measure the amount of triglycerides in your blood. Triglycerides are a type of fat.
Your body makes some triglycerides. Triglycerides also come from the food you eat. Extra calories are turned into triglycerides and stored in fat cells for later use.
A test for high blood cholesterol levels is a related measurement and usually done at the same time.
-
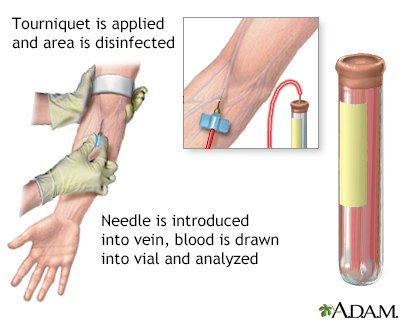
How the Test is Performed
A blood sample is needed. Most of the time, blood is drawn from a vein located on the inside of the elbow or the back of the hand.
-
How to Prepare for the Test
You should not eat for 8 to 12 hours before the test.
Alcohol and some medicines can interfere with blood test results.
- Make sure your health care provider knows what medicines you take, including over-the-counter drugs and supplements.
- Your provider will tell you if you need to stop taking any medicines before you have this test.
- Do not stop or change your medicines without talking to your provider first.
-
Why the Test is Performed
Triglycerides are usually measured together with other blood fats. Often it is done to help determine your risk of developing heart disease. A high triglyceride level may lead to atherosclerosis, which increases your risk for heart attack and stroke.
A very high triglyceride level may also cause inflammation of your pancreas (called pancreatitis).
-
Normal Results
Results may indicate:
- Normal: Less than 150 mg/dL (1.69 mmol/L)
- Borderline high: 150 to 199 mg/dL (1.69 to 2.25 mmol/L)
- High: 200 to 499 mg/dL (2.26 to 5.64 mmol/L)
- Very high: 500 mg/dL or above (5.65 mmol/L)
Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test results.
The examples above show the common measurements for results for these tests. Some laboratories use different measurements or may test different specimens.
-
What Abnormal Results Mean
High triglyceride levels may be due to:
- Cirrhosis or liver damage
- Diet low in protein and high in carbohydrates
- Underactive thyroid
- Nephrotic syndrome (a kidney disorder)
- Other medicines, such as female hormones
- Poorly controlled diabetes
- Disorder passed down through families in which there are high amounts of cholesterol and triglycerides in the blood
Overall, the treatment of elevated triglyceride levels focuses on increased exercise and changes in the diet. Drugs to lower triglyceride levels may be used to prevent pancreatitis for levels above 500 mg/dL.
Low triglyceride levels may be due to:
- Low fat diet
- Hyperthyroidism (overactive thyroid)
- Malabsorption syndrome (conditions in which the small intestine does not absorb fats well)
- Malnutrition
-
Considerations
Pregnancy can affect test results.
References
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Bredefeld CL, Lau R, Hussain MM. Lipids and dyslipoproteinemia. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 18.
Genest J, Mora S, Libby P. Lipoprotein disorders and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli, GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 27.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1046-e1081. PMID: 30565953 pubmed.ncbi.nlm.nih.gov/30565953/.
Kakavand H, Aghakouchakzadeh M, Shahi A, et al. A stepwise approach to prescribing novel lipid-lowering medications. J Clin Lipidol. 2022;16(6):822-832. PMID: 36522804 pubmed.ncbi.nlm.nih.gov/36522804/.
Mora S, Libby P, Ridker PM. Risk markers and the primary prevention of cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 25.
Robinson JG. Disorders of lipid metabolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 190.