Medicines for osteoporosis
Alendronate (Fosamax); Ibandronate (Boniva); Risedronate (Actonel); Zoledronic acid (Reclast); Raloxifene (Evista); Teriparatide (Forteo); Denosumab (Prolia); Romosozumab (Evenity); Low bone density - medicines; Osteoporosis - medicinesOsteoporosis is a disease that causes bones to become brittle and more likely to fracture (break). With osteoporosis, the bones lose density. Bone density is the amount of calcified bone tissue that is in your bones.
Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).

When are Medicines Used?
Your health care provider may prescribe certain medicines to help lower your risk of fractures. These medicines can make the bones in your hips, spine, and other areas less likely to break.
Your provider may prescribe medicines when:
- A bone density test shows you have osteoporosis, even if you have not had a fracture before, but your fracture risk is high.
Bone density test
A bone mineral density (BMD) test measures how much calcium and other types of minerals are in an area of your bone. This test helps your health care...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You have a bone fracture, and a bone density test shows you have a bone density lower than normal, but not osteoporosis.
- You have a bone fracture that occurs without any significant injury.
Bisphosphonates
Bisphosphonates are the main medicines that are used to both prevent and treat bone loss. They are most often taken by mouth. You may take a pill once daily, weekly, or monthly. You also may get bisphosphonates through a vein (IV). Most often this is done once or twice a year.
Common side effects with bisphosphonates taken by mouth are heartburn, nausea, and pain in the belly. When you take bisphosphonates:
- Take them on an empty stomach in the morning with 6 to 8 ounces (oz), or 180 to 240 milliliters (mL), of plain water (not carbonated water or juice).
- After taking the pill, remain sitting or standing for at least 30 minutes.
- Do not eat or drink for at least 30 to 60 minutes.
Rare side effects are:
- Low blood calcium level
- A certain type of leg-bone (femur) fracture
- Damage to the jaw bone
- Fast, abnormal heartbeat (atrial fibrillation)
Your provider may have you stop taking this medicine after about 5 years. Doing so decreases the risk of certain side effects. This is called a medicine holiday.
Other Drugs for Osteoporosis
Raloxifene (Evista) may also be used to prevent and treat osteoporosis.
- It can reduce the risk of spinal fractures, but not other types of fractures.
- The most serious side effect is a very small risk of blood clots in the leg veins or in the lungs.
Blood clots in the leg veins
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. DVT mainly affects the large...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleIn the lungs
A pulmonary embolus is a blockage of an artery in the lungs. The most common cause of the blockage is a blood clot.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - This medicine may also help decrease the risk of heart disease and breast cancer.
- Other selective estrogen receptor modulators (SERMs) are also used to treat osteoporosis.
Denosumab (Prolia) is a medicine that prevents bones from becoming more fragile. This medicine:
- Is given as an injection every 6 months.
- May increase bone density more than bisphosphonates.
- Is generally not a first-line treatment.
- May not be a good choice for people who have weak immune systems or who take medicines that affect the immune system.
Teriparatide (Forteo) is a bio-engineered form of parathyroid hormone. This medicine:
- May increase bone density and decrease the risk for fractures.
- Is given as an injection underneath the skin at home, often every day.
- Does not seem to have severe long-term side effects, but may cause nausea, dizziness, or leg cramps.
Estrogen, or hormone replacement therapy (HRT). This medicine:
- Is very effective in preventing and treating osteoporosis.
- Was the most commonly used osteoporosis medicine for many years. Its use decreased because of concern that this medicine caused heart disease, breast cancer, and blood clots.
- Is still a good option for many younger women (50 to 60 years old). If a woman is taking estrogen already, she and her provider must discuss the risks and benefits of doing so.
Romosozumab (Evenity) targets a hormone pathway in bone called sclerostin. This medicine:
- Is given monthly as an injection under the skin for one year.
- Is effective at increasing bone density.
- May make calcium levels too low.
- May possibly increase the risk of heart attack and stroke.
Parathyroid hormone
- This medicine is given as daily shots under the skin. Your provider or nurse will teach you how to give yourself these shots at home.
- Parathyroid hormone works better if you have never taken bisphosphonates.
Calcitonin is a medicine that slows the rate of bone loss. This medicine:
- Is sometimes used after a bone fracture because it decreases bone pain.
- Is much less effective than bisphosphonates.
- Comes as a nasal spray or an injection.
When to Call the Doctor
Contact your provider for these symptoms or side effects:
- Chest pain, heartburn, or problems swallowing
- Nausea and vomiting
- Blood in your stool
- Swelling, pain, redness in one of your legs
- Fast heart beat
- Skin rash
- Pain in your thigh or hip
- Pain in your jaw
References
De Paula FJA, Black DM, Rosen CJ. Osteoporosis: basic and clinical aspects. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 30.
Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104(5):1595-1622. PMID: 30907953 pubmed.ncbi.nlm.nih.gov/30907953/.
Weber TJ. Osteoporosis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 225.
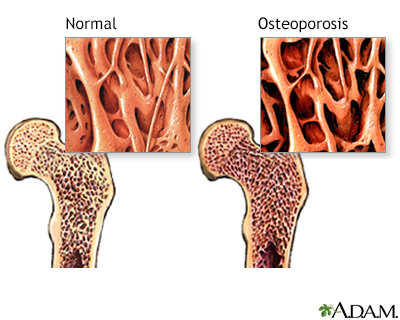
Osteoporosis - illustration
The bone disease osteoporosis is caused by more bone matrix being resorbed than being deposited. This imbalance results in a progressive loss of bone density and a thinning of bone tissue. Osteoporotic bones are more porous and therefore more vulnerable to fracture.
Osteoporosis
illustration
Osteoporosis - illustration
The bone disease osteoporosis is caused by more bone matrix being resorbed than being deposited. This imbalance results in a progressive loss of bone density and a thinning of bone tissue. Osteoporotic bones are more porous and therefore more vulnerable to fracture.
Osteoporosis
illustration
Review Date: 5/20/2024
Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.