Heart failure - home monitoring
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptoms to occur throughout the body. Watching out for the warning signs that your heart failure is getting worse may help you catch problems before they become too serious.
Heart failure - Animation
If you cough a lot, often feel weak, have lost your appetite, and need to urinate a lot at night, you might have symptoms of heart failure. Heart failure is a long-term condition that usually comes on slowly. However, it can develop suddenly, for instance, after a heart attack. You have heart failure when your heart does not pump blood out of your heart very well, or when your heart muscles are stiff and do not easily fill up with blood. When you have heart failure, your heart cannot pump enough oxygen-rich blood to the rest of your body, especially when you exercise or move around a lot. As the heart loses the ability to pump blood, blood backs up in other parts of your body, including your lungs, liver, gastrointestinal tract, and your arms and legs. The most common cause of heart failure is coronary artery disease, the narrowing of the blood vessels that supply blood and oxygen to your heart. So, how do you know if you have heart failure? Get to your doctor. You may have trouble breathing, an irregular heartbeat, swollen legs, neck veins that stick out, and sounds from fluid built up in your lungs. Your doctor will check for these and other signs of heart failure. A test called an echocardiogram is often the best test to diagnose your heart failure. Your doctor can also use this test to find out why you have heart failure, and then monitor your condition going forward every three to six months. Your doctor will talk to you about knowing your body and symptoms that mean your heart failure is getting worse. You will need to learn to watch for changes in your heart rate, pulse, blood pressure, and weight. You will also need to limit salt in your diet, stop drinking alcohol, quit smoking if you need to, exercise, lose weight if you need to, and get enough rest. Your doctor will probably ask you to take medicines to treat your heart failure. These medicines can treat your symptoms, prevent your heart failure from getting worse, and help you live longer. If you have heart failure, taking your medicines, changing your lifestyle, and treating the condition that caused heart failure can go a long way toward improving your health. But heart failure is a chronic, or long-term, illness, which means it may get worse over time. Make sure you call your doctor if you start coughing more, have sudden weight gain or swelling, or feel week. Have someone take you to the emergency room right away if you have trouble with fainting, a fast and irregular heartbeat, or feel severe crushing chest pain.
What to Expect at Home
Knowing your body and the symptoms that tell you your heart failure is getting worse will help you stay healthier and out of the hospital. At home, you should watch for changes in your:
- Blood pressure
- Heart rate
- Pulse
- Weight
By watching out for warning signs, you can catch problems before they get too serious. Sometimes these simple checks will remind you that you forgot to take a pill, or that you have been drinking too much fluid or eating too much salt.
Be sure to write down the results of your home self-checks so that you can share them with your health care provider. Your provider's office may have a "telemonitor," a device you can use to send your information automatically. A nurse will go over your self-check results with you in a regular (sometimes weekly) phone call.
Throughout the day, ask yourself:
- Is my energy level normal?
- Am I getting more short of breath when I am doing my everyday activities?
- Are my clothes or shoes feeling tight?
- Are my ankles or legs swelling?
- Am I coughing more often? Does my cough sound wet?
- Do I get short of breath at night?
These are signs that there is too much fluid building up in your body. You will need to learn how to limit your fluids and salt intake to prevent these things from happening.
Your fluids
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes fluid t...
Read Article Now Book Mark ArticleSalt intake
Too much sodium in your diet can be bad for you. If you have high blood pressure or heart failure, you may be asked to limit the amount of salt (whi...

Checking Your Weight
You will get to know what weight is right for you. Weighing yourself will help you know if there is too much fluid in your body. You might also find that your clothes and shoes are feeling tighter than normal when there is too much fluid in your body.
Weigh yourself every morning on the same scale when you get up -- before you eat and after you use the bathroom. Make sure you are wearing similar clothing each time you weigh yourself. Write down your weight every day on a chart so that you can keep track of it.
Contact your provider if your weight goes up by more than 2 to 3 pounds (1 to 1.5 kilograms, kg) in a day or 5 pounds (2 kilograms) in a week. Also contact your provider if you lose a lot of weight.
Checking Your Heart Rate and Pulse
Know what your normal pulse rate is. Your provider will tell you what yours should be.
You can take your pulse in the wrist area below the base of your thumb. Use your index and third fingers of your other hand to find your pulse. Use a second hand and count the number of beats for 30 seconds. Then double that number. That is your pulse.
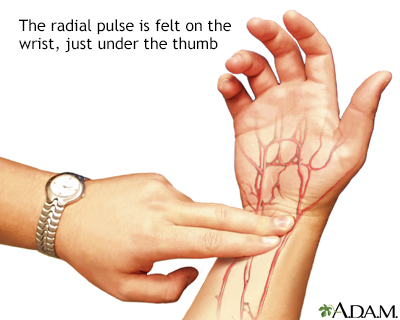
Radial pulse
Arteries carry oxygenated blood away from the heart to the tissues of the body. Veins carry blood depleted of oxygen from the same tissues back to the heart. The arteries are the vessels with the pulse, a rhythmic pushing of the blood in the heart followed by a refilling of the heart chamber. To determine heart rate, one counts the beats at a pulse point like the inside of the wrist for 10 seconds, and multiplies this number by 6. This is the per-minute total.
Your provider may give you special equipment to check your heart rate.
Checking Your Blood Pressure
Your provider may ask you to keep track of your blood pressure at home. Make sure you get a good quality, well-fitting home device. Show it to your provider or nurse. It will probably have a cuff with a stethoscope or a digital readout.
Practice with your provider to make sure you are taking your blood pressure correctly.
Blood pressure - Animation
The force of blood on artery walls is called blood pressure. Normal pressure is important for the proper flow of blood from the heart to the body's organs and tissues. Each heart beat forces blood to the rest of the body. Near the heart, pressure is higher, and away from it lower. Blood pressure depends on many things, including how much blood the heart is pumping and the diameter of the arteries the blood is moving through. Generally, the more blood that's pumped and the narrower the artery the higher the pressure is. Blood pressure is measured both as the heart contracts, which is called systole, and as it relaxes, which is called diastole. Systolic blood pressure is measured when the heart ventricles contract. Diastolic blood pressure is measured when the heart ventricles relax. A systolic pressure of 115 millimeters of mercury is considered normal, as is a diastolic pressure of 70. Commonly, this pressure would be stated as 115 over 70. Stressful situations can temporarily cause blood pressure to rise. If a person has a consistent blood pressure reading of 140 over 90, he would be evaluated for high blood pressure. Left untreated, high blood pressure can damage important organs, such as the brain and kidneys, as well as lead to a stroke.
When to Call the Doctor
Contact your provider if:
- You are tired or weak.
- You feel short of breath when you are active or when you are at rest.
- You have shortness of breath when you lie down, or an hour or two after falling asleep.
- You are wheezing and having trouble breathing.
- You have a cough that does not go away. It may be dry and hacking, or it may sound wet and bring up pink, foamy spit.
- You have swelling in your feet, ankles, or legs.
- You have to urinate a lot, particularly at night.
- You have gained or lost weight.
- You have pain or tenderness in your belly.
- You have symptoms you think might be from your medicines.
- Your pulse or heartbeat gets very slow or very fast, or it is not regular.
- Your blood pressure is lower or higher than is normal for you.
Reviewed By
Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Heidenreich PA, Bozkurt B, Aguilar D, 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;146(13):e185. PMID: 35363499 pubmed.ncbi.nlm.nih.gov/35363499/.
Lam CSP, Shah SJ, Solomon SD. Heart failure with preserved and mildly reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 51.
Mann DL. Management of heart failure patients with reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 50.


 All rights reserved.
All rights reserved.