Heart attack – discharge
Myocardial infarction - discharge; MI - discharge; Coronary event - discharge; Infarct - discharge; Acute coronary syndrome - discharge; ACS - dischargeA heart attack occurs when blood flow to a part of your heart is blocked long enough that part of the heart muscle is damaged or dies. This article discusses what you need to do to take care of yourself after you leave the hospital.
When You're in the Hospital
You were in the hospital because you had a heart attack. A heart attack occurs when blood flow to a part of your heart is blocked long enough that part of the heart muscle is damaged or dies.
Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...

What to Expect at Home
You may feel sad. You may feel anxious and as though you have to be very careful about what you do. All of these feelings are normal. They go away for most people after 2 or 3 weeks. You may also feel tired when you leave the hospital to go home.
Activity
You should know the signs and symptoms of angina.
- You may feel pressure, squeezing, burning, or tightness in your chest. You may also notice these symptoms in your arms, shoulders, neck, jaw, throat, or back.
- Some people also feel discomfort in their back, shoulders, and stomach area.
- You may have indigestion or feel sick to your stomach.
- You may feel tired and be short of breath, sweaty, lightheaded, or weak.
- You may have angina during physical activity, such as climbing stairs or walking uphill, lifting, sexual activity, or when you are out in cold weather. It can also happen when you are resting or it can wake you up when you are sleeping.
Angina
Angina is a type of chest discomfort or pain due to poor blood flow through the blood vessels (coronary arteries) of the heart muscle (myocardium). ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Know how to treat your chest pain when it happens. Talk with your health care provider about what to do.
How to treat your chest pain when it ha...
Angina is a type of chest discomfort due to poor blood flow through the blood vessels of the heart muscle. This article discusses how to care for yo...
Read Article Now Book Mark ArticleTake it easy for the first 4 to 6 weeks after your heart attack.
- Avoid heavy lifting. Get some help with household chores if you can.
- Take 30 to 60 minutes to rest in the afternoon for first 4 to 6 weeks. Try to go to bed early and get plenty of sleep.
- Before starting to exercise, your provider may have you do an exercise test and recommend an exercise plan. This may happen before you leave the hospital or soon afterward. Do not change your exercise plan before talking with your provider.
Starting to exercise
A heart attack occurs when blood flow to a part of your heart is blocked long enough that part of the heart muscle is damaged or dies. Starting a re...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Your provider may refer you to cardiac rehabilitation program. There, you will learn how to slowly increase your exercise and how to take care of your heart disease.
- If you had angiography, follow your provider's instructions to care for the puncture site.
You should be able to talk comfortably when you are doing any activity, such as walking, setting the table, and doing laundry. If you cannot, stop the activity.
Ask your provider about when you can return to work. Expect to be away from work for at least a week.
Talk to your provider before engaging in sexual activity. Ask your provider when it is OK to start again. Do not take Viagra, Levitra, Cialis or any herbal remedy for erection problems without checking with your provider first.
How long you will have to wait to return to your normal activities will depend on:
- Your physical condition before your heart attack
- The size of your heart attack
- If you had complications
- The overall speed of your recovery
Diet and Lifestyle
Do not drink any alcohol for at least 2 weeks. Ask your provider when you may start and for other guidance about how much alcohol is safe for you.
If you smoke, stop. Ask your provider for help quitting if you need it. Do not let anybody smoke in your home, since second-hand smoke can harm you. Try to stay away from things that are stressful for you. If you are feeling stressed all the time, or if you are feeling very sad, talk with your provider. They can refer you to a counselor.
Learn more about what you should eat to make your heart and blood vessels healthier.
- Avoid salty foods.
Salty
Too much sodium in your diet can be bad for you. If you have high blood pressure or heart failure, you may be asked to limit the amount of salt (whi...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Stay away from fast food restaurants.
Fast food
Many fast foods are high in calories, fat, salt, and sugar. Use these tips to guide you in making healthier choices when eating in a fast food resta...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Taking Your Heart Medicines
Have your prescriptions filled before you go home. It is very important that you take your medicines the way your provider told you to. Do not take any other medicines or herbal supplements without asking your provider first if they are safe for you.
Take your medicines with water. Do not take them with grapefruit juice, since it may change how your body absorbs certain medicines. Ask your provider or pharmacist for more information about this.
The medicines below are given to most people after they have had a heart attack. Sometimes there is a reason they may not be safe to take, though. These medicines help prevent another heart attack. Talk with your provider if you are not already on any of these medicines:
- Antiplatelets medicines (blood thinners), such as aspirin, clopidogrel (Plavix), warfarin (Coumadin), prasugrel (Efient), or ticagrelor (Brilinta) to help keep your blood from clotting
Aspirin
Current guidelines recommend that people with coronary artery disease (CAD) receive antiplatelet therapy with either aspirin or clopidogrel. Aspirin ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleClopidogrel
Platelets are small particles in your blood that your body uses to form clots and stop bleeding. If you have too many platelets or your platelets st...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleWarfarin
Warfarin is a medicine that makes your blood less likely to form clots. It is important that you take warfarin exactly as you have been told. Chang...
Read Article Now Book Mark Article - Beta-blockers and ACE inhibitor medicines to help protect your heart
ACE inhibitor
Angiotensin-converting enzyme (ACE) inhibitors are medicines. They treat heart, blood vessel, and kidney problems.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Statins or other drugs to lower your cholesterol
Statins or other drugs to lower your ch...
Your body needs cholesterol to work properly. But extra cholesterol in your blood causes deposits to build up on the inside walls of your blood vess...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Calcium-channel blockers
- Nitroglycerin
Do not suddenly stop taking these medicines for your heart. Do not stop taking medicines for your diabetes, high blood pressure, or any other medical conditions you may have without talking with your provider first.
If you are taking a blood thinner such as warfarin (Coumadin), you may need to have extra blood tests on a regular basis to make sure your dose is correct.
When to Call the Doctor
Contact your provider if you feel:
- Pain, pressure, tightness, or heaviness in your chest, arm, neck, or jaw
- Shortness of breath
- Gas pains or indigestion
- Numbness in your arms
- Sweaty, or if you lose color
- Lightheaded
Changes in your angina may mean your heart disease is getting worse. Contact your provider if your angina:
- Becomes stronger
- Happens more often
- Lasts longer
- Occurs when you are not active or when you are resting
- Medicines do not help ease your symptoms as well as they used to
References
Bohula EA, Morrow DA. ST-elevation myocardial infarction: management. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 38.
Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 39.
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: executive summary: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454. PMID: 34709928 pubmed.ncbi.nlm.nih.gov/34709928/.
Kumbhani DJ, Bhatt DL. Percutaneous coronary intervention. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 41.
Morrow DA, de Lemos J. Stable ischemic heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 40.
-
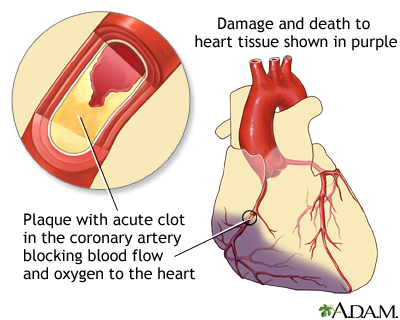
Acute MI - illustration
A heart attack or acute myocardial infarction (MI) occurs when one of the arteries that supplies the heart muscle becomes blocked. Blockage may be caused by spasm of the artery or by atherosclerosis with acute clot formation. The blockage results in damaged tissue and a permanent loss of contraction of this portion of the heart muscle.
Acute MI
illustration
-
Acute MI - illustration
A heart attack or acute myocardial infarction (MI) occurs when one of the arteries that supplies the heart muscle becomes blocked. Blockage may be caused by spasm of the artery or by atherosclerosis with acute clot formation. The blockage results in damaged tissue and a permanent loss of contraction of this portion of the heart muscle.
Acute MI
illustration
-
Heart attack and acute coronary syndrome - InDepth
(In-Depth)
-
Menopause - InDepth
(In-Depth)
-
Migraine headaches - InDepth
(In-Depth)
-
Hypothyroidism - InDepth
(In-Depth)
-
Gallstones and gallbladder disease - InDepth
(In-Depth)
-
Smoking - InDepth
(In-Depth)
-
Pneumonia - InDepth
(In-Depth)
-
Pelvic inflammatory disease
(Alt. Medicine)
-
Burns
(Alt. Medicine)
-
Hodgkin disease - InDepth
(In-Depth)
Review Date: 8/5/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.