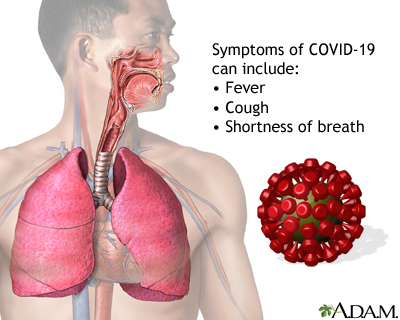
COVID-19 symptoms
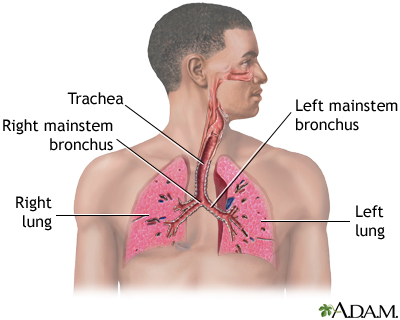
COVID-19 is a highly infectious respiratory illness caused by a virus called SARS-CoV-2.
COVID-19 symptoms can range from mild to severe. Symptoms may include:
- Fever
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chills
- Cough
Cough
Coughing is an important way to keep your throat and airways clear. But too much coughing may mean you have a disease or disorder. Some coughs are d...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Coughing up blood (hemoptysis)
- Shortness of breath or difficulty breathing
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fatigue
- Muscle aches
Muscle aches
Muscle aches and pains are common and can involve more than one muscle. Muscle pain also can involve ligaments, tendons, and fascia. Fascias are th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Headache
- Loss of sense of taste or smell
- Sore throat
- Stuffy or runny nose
- Nausea and vomiting
- Diarrhea
This is not a complete list of possible symptoms. Symptoms may change with new variants of the virus.
Some people may have no symptoms at all. Many have only some, but not all of the symptoms. Symptoms can also vary, depending on whether you are vaccinated.
Symptoms may develop within 2 to 14 days after you are exposed to the virus. Most often, symptoms appear around 5 days after exposure. However, you can spread the virus even when you do not have symptoms.
More severe symptoms that require seeking medical help right away include:
- Trouble breathing
- Chest pain or pressure that persists
- Confusion
- Inability to wake up
- Blue, gray, or pale skin, lips, face, or nail beds (cyanosis), depending on your skin tone
Cyanosis
A bluish color to the skin or mucous membrane is usually due to a lack of oxygen in the blood. The medical term is cyanosis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Older people and people with certain existing health conditions have a higher risk of developing severe illness and death. Health conditions that increase your risk include cancer, COPD, diabetes, heart disease and stroke, a weak immune system (immunocompromised), and many others.
Cancer
Cancer is the uncontrolled growth of abnormal cells in the body. Cancerous cells are also called malignant cells.
Read Article Now Book Mark ArticleCOPD
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe. There are two main forms of COPD:Chroni...

Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...

Considerations
Some symptoms of COVID-19 are similar to those of the common cold and the flu, so it can be hard to know for sure if you have the SARS-CoV-2 virus. But COVID-19 is not a cold, and it is not a flu.
COVID-19
Coronavirus disease 2019 (COVID-19) is a respiratory illness that causes fever, coughing, and shortness of breath, but many other symptoms can occur....

The only way to know if you have COVID-19 is to be tested. If you want to be tested, you should contact your health care provider or use a home diagnostic test.
Tested
Testing for the virus that causes COVID-19 involves taking a mucus sample from your upper respiratory tract. This test is used to diagnose COVID-19....

Home diagnostic test
Self-testing for COVID-19 can be done using an over-the-counter (OTC) rapid antigen test to find out if you have COVID-19 infection. An OTC test for...

Most people with the illness have mild to moderate symptoms and recover fully. Whether you get tested or not, if you have symptoms of COVID-19, you should avoid contact with other people so you don't spread the illness.
Causes
COVID-19 is caused by the SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2). Coronaviruses are a family of viruses that can affect people and animals. They can cause mild to severe respiratory illnesses.
Coronaviruses
Coronaviruses are a family of viruses. Infection with these viruses generally causes mild to moderate respiratory illnesses, such as the common cold...

COVID-19 spreads to people within close contact (about 6 feet or 2 meters). When someone with the illness coughs or sneezes, infectious droplets spray into the air. You can catch the illness if you breathe in or touch these particles and then touch your face, nose, mouth, or eyes.
Home Care
If you have COVID-19 or think you have it, stay at home and avoid contact with other people, both inside and outside your home, to avoid spreading the illness. You should do this right away and not wait for any COVID-19 testing.
Stay at home and avoid contact with oth...
Staying at home when you have COVID-19 helps protect other people who are not infected with the virus. You should stay at home and away from other p...

Avoid spreading the illness
Coronavirus disease 2019 (COVID-19) is a serious disease, mainly of the respiratory system, affecting many people around the globe. It can cause mil...

To help treat the symptoms of COVID-19, the following tips may help.
Treat the symptoms of COVID-19
You have recently been diagnosed with coronavirus disease 2019 (COVID-19). COVID-19 causes an infection in your lungs and may cause problems with ot...

- Rest and drink plenty of fluids.
- Acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) help reduce fever. Sometimes, providers advise you to use both types of medicine. Take the recommended amount to reduce fever. Do not use ibuprofen in children 6 months or younger.
- A lukewarm bath or sponge bath may help cool a fever. Keep taking medicine -- otherwise your temperature might go back up.
- If you have a dry, tickling cough, try cough drops or hard candy.
- Use a vaporizer or take a steamy shower to increase moisture in the air and help soothe a dry throat and cough.
- Do not smoke, and stay away from secondhand smoke.
When to Contact a Medical Professional
You should contact your provider right away:
- If you have symptoms and think you may have COVID-19
- If you have COVID-19 and you are in a group for whom antiviral medicine may be given
- If you have COVID-19 and your symptoms are getting worse
Call 911 or the local emergency number if you have:
- Trouble breathing
Trouble breathing
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chest pain or pressure that persists
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Confusion or inability to wake up
- Blue, gray, or pale skin, lips, face, or nail beds (cyanosis)
- Any other symptoms that are severe or that concern you
What to Expect at Your Office Visit
Your provider will ask about your symptoms, any recent travel, and any possible exposure to COVID-19. Your provider may take swab samples from the back of your nose and throat.
If your symptoms do not indicate a medical emergency, you can recover at home.
For more serious symptoms, you may need to go to the hospital for care.
Hospital for care
You have been in the hospital with COVID-19, which causes an infection in your lungs and may cause problems with other organs, including the kidneys,...

Reviewed By
Linda J. Vorvick, MD, Clinical Professor Emeritus, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 06/05/2025.
Centers for Disease Control and Prevention website. COVID-19: testing for COVID-19. www.cdc.gov/covid/testing/index.html. Updated March 10, 2025. Accessed June 5, 2025.
Centers for Disease Control and Prevention website. COVID-19: types of COVID-19 treatment. www.cdc.gov/covid/treatment/index.html. Updated May 8, 2025. Accessed June 5, 2025.
Centers for Disease Control and Prevention website. Respiratory illnesses: respiratory virus guidance. www.cdc.gov/respiratory-viruses/guidance/index.html. Updated March 1, 2024. Accessed January 3, 2025.
Centers for Disease Control and Prevention website. COVID-19: symptoms of COVID-19. www.cdc.gov/covid/signs-symptoms/index.html. Updated March 10, 2025. Accessed June 5, 2025.
Del Rio C, Gandhi M, Cohen MS. COVID-19: epidemiology, clinical manifestations, diagnosis, and community prevention. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 336.





 All rights reserved.
All rights reserved.