COVID-19 virus test
COVID-19 - Nasopharyngeal swab; SARS CoV-2 test; COVID-19 PCR testTesting for the virus that causes COVID-19 involves taking a mucus sample from your upper respiratory tract. This test is used to diagnose COVID-19.
The COVID-19 virus test is not used to test your immunity to COVID-19. To test if you have antibodies against the SARS-CoV-2 virus, you need a COVID-19 antibody test taken from a blood sample.
COVID-19 antibody test
This blood test shows if you have antibodies against the virus that causes COVID-19. Antibodies are proteins produced by the body in response to ha...

How the Test is Performed
Testing is usually done in one of two ways. For a nasopharyngeal test, you will be asked to tilt your head back slightly. A sterile, cotton-tipped swab is gently passed through a nostril and into the nasopharynx. This is the uppermost part of the throat, behind the nose. The swab is left in place for several seconds, rotated, and removed. This same procedure may be done on your other nostril.
For an anterior nasal test, the swab will be inserted into your nostril no more than 3/4 of an inch (2 centimeters). The swab will be rotated at least 4 times while pressing against the inside of your nostril. The same swab will be used to collect samples from both nostrils.
Tests may be done by a health care provider at an office, drive-through, or walk-up location. Check with your local health department to find out where testing is available in your area.
At-home testing kits (self-tests) are available over-the-counter. Most kits have you collect a sample using a nasal swab, and you can get results at home in minutes. Be sure to follow the instructions that come with the kit,
At-home testing
Self-testing for COVID-19 can be done using an over-the-counter (OTC) rapid antigen test to find out if you have COVID-19 infection. An OTC test for...

There are two types of virus tests available that can diagnose COVID-19:
- Polymerase chain reaction (PCR) tests (also called Nucleic Acid Amplification Tests [NAATs]) detect the genetic material of the virus that causes COVID-19. The samples are usually sent to a lab for testing, and results are usually available in 1 to 3 days. There are also rapid PCR diagnostic tests that are run on specialized equipment on-site, for which the results are available in several minutes. PCR tests tend to be the most reliable tests, whether or not you have symptoms.
- Antigen tests detect specific proteins on the virus that causes COVID-19. Antigen tests are rapid diagnostic tests, which means results are available in several minutes. Self-tests taken at home are antigen tests. These tests are not as reliable as PCR tests, especially if you do not have symptoms.
- Rapid diagnostic tests of any kind are less accurate than the regular PCR test. If you get a negative result on a rapid test, but have symptoms of COVID-19, your provider may do a non-rapid PCR test.
How to Prepare for the Test
No special preparation is needed.
How the Test will Feel
Depending on the type of test, you may have slight or moderate discomfort, your eyes may water, and you may gag.
Why the Test is Performed
The test identifies the SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2), which causes COVID-19.
COVID-19
Coronavirus disease 2019 (COVID-19) is a respiratory illness that causes fever, coughing, and shortness of breath, but many other symptoms can occur....

Normal Results
The test is considered normal when it is negative. A negative test means that at the time you were tested, you probably didn't have the virus that causes COVID-19 in your respiratory tract. But you can test negative if you were tested too early after infection for the SARS-CoV-2 virus to be detected. And you can have a positive test later if you are exposed to the virus after you were tested. Also, rapid diagnostic tests of any kind are less accurate than the regular PCR test, and either test may remain positive for weeks after you've recovered from the illness.
For this reason, if you have symptoms of COVID-19 or you are at risk for contracting COVID-19 and your first test result was negative, your provider may recommend being retested at a later time. A single negative self-test will not rule out infection. If you used a self-test, you should take at least one more test again in 48 hours. Take a third test 48 hours after the second test if you don't have symptoms. Or, your provider may recommend a PCR test to confirm your results.
What Abnormal Results Mean
A positive test means that you are infected with SARS-CoV-2. You may or may not have symptoms of COVID-19, the illness caused by the virus. Whether you have symptoms or not, you can still spread the illness to others. You should stay at home away from others until your symptoms are better, and you are free of fever for at least 24 hours (without taking fever-reducing medicine). Continue to take precautions for another 5 days to protect others from developing COVID-19.
Symptoms of COVID-19
COVID-19 is a highly infectious respiratory illness caused by a virus called SARS-CoV-2. COVID-19 symptoms can range from mild to severe. Symptoms m...

Stay at home away from others
Staying at home when you have COVID-19 helps protect other people who are not infected with the virus. You should stay at home and away from other p...

References
Centers for Disease Control and Prevention website. COVID-19: Interim guidelines for collecting and handling of clinical specimens for COVID-19 testing. www.cdc.gov/covid/hcp/clinical-care/clinical-specimen-guidelines.html. Updated October 29, 2024. Accessed January 6, 2025.
Centers for Disease Control and Prevention website. COVID-19: testing for COVID-19. www.cdc.gov/covid/testing/index.html. Updated March 10, 2025. Accessed June 5, 2025.
Del Rio C, Gandhi M, Cohen MS. COVID-19: epidemiology, clinical manifestations, diagnosis, and community prevention. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 336.
US Food and Drug Administration website. COVID-19 test basics. www.fda.gov/consumers/consumer-updates/covid-19-test-basics. Updated September 7, 2023. Accessed January 6, 2025.
COVID-19 - illustration
Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19, a respiratory illness that ranges from mild symptoms to pneumonia or even death. Symptoms occur within 2 to 14 days from exposure to the virus and may include fever, cough, shortness of breath, chills, muscle pain, headache, sore throat, and new loss of sense of taste or smell. COVID-19 may be more severe in people who are older or who have chronic health conditions, such as heart disease or diabetes.
COVID-19
illustration
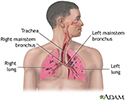
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Upper respiratory tract - illustration
The major passages and structures of the upper respiratory tract include the nose or nostrils, nasal cavity, mouth, throat (pharynx), and voice box (larynx). The respiratory system is lined with a mucous membrane that secretes mucus. The mucus traps smaller particles like pollen or smoke. Hairlike structures called cilia line the mucous membrane and move the particles trapped in the mucus out of the nose. Inhaled air is moistened, warmed, and cleansed by the tissue that lines the nasal cavity.
Upper respiratory tract
illustration
COVID-19 - illustration
Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes COVID-19, a respiratory illness that ranges from mild symptoms to pneumonia or even death. Symptoms occur within 2 to 14 days from exposure to the virus and may include fever, cough, shortness of breath, chills, muscle pain, headache, sore throat, and new loss of sense of taste or smell. COVID-19 may be more severe in people who are older or who have chronic health conditions, such as heart disease or diabetes.
COVID-19
illustration
Respiratory system - illustration
Air is breathed in through the nasal passageways, travels through the trachea and bronchi to the lungs.
Respiratory system
illustration
Upper respiratory tract - illustration
The major passages and structures of the upper respiratory tract include the nose or nostrils, nasal cavity, mouth, throat (pharynx), and voice box (larynx). The respiratory system is lined with a mucous membrane that secretes mucus. The mucus traps smaller particles like pollen or smoke. Hairlike structures called cilia line the mucous membrane and move the particles trapped in the mucus out of the nose. Inhaled air is moistened, warmed, and cleansed by the tissue that lines the nasal cavity.
Upper respiratory tract
illustration
Review Date: 1/1/2025
Reviewed By: Linda J. Vorvick, MD, Clinical Professor Emeritus, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 06/05/2025.