Stress echocardiography
Echocardiography stress test; Stress test - echocardiography; CAD - stress echocardiography; Coronary artery disease - stress echocardiography; Chest pain - stress echocardiography; Angina - stress echocardiography; Heart disease - stress echocardiographyStress echocardiography is a test that uses ultrasound imaging to show how well your heart muscle is working to pump blood to your body while you exercise in a controlled setting. It is most often used to detect a decrease in blood flow to the heart muscle due to narrowing in the coronary arteries.
Narrowing in the coronary arteries
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...

How the Test is Performed
This test is done at a medical center or health care provider's office.
A resting echocardiogram will be done first. While you lie on your left side with your left arm out, a small device called a transducer is held against your chest. A special gel is used to help the ultrasound waves get to your heart.
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...

Most people will walk on a treadmill (or pedal on an exercise bicycle). Slowly (about every 3 minutes), you will be asked to walk (or pedal) faster and on an incline. It is like being asked to walk fast or jog up a hill.
In most cases, you will need to walk or pedal for 5 to 15 minutes, depending on your level of fitness and your age. Your provider will ask you to stop:
- When your heart is beating at the target rate
- When you are too tired to continue
- If you are having chest pain or a change in your blood pressure that worries the provider administering the test
If you are not able to exercise, you will get a drug, such as dobutamine, through a vein (intravenous line). This medicine will make your heart beat faster and harder, similar to when you exercise.
Your blood pressure and heart rhythm (ECG) will be monitored throughout the procedure.
More echocardiogram images will be taken while your heart rate is increasing, or when it reaches its peak. The images will show whether any parts of your heart muscle do not work as well when your heart rate increases. This is a sign that part of the heart may not be getting enough blood or oxygen because of narrowed or blocked arteries.
How to Prepare for the Test
Ask your provider if you should take any of your normal medicines on the day of the test. Some medicines may interfere with test results. Never stop taking any medicine without first talking to your provider.
It is important to tell your provider if you have taken any of the following medicines within the past 24 hours (1 day):
- Sildenafil citrate (Viagra)
- Tadalafil (Cialis)
- Vardenafil (Levitra)
DO NOT eat or drink for at least 3 hours before the test.
Wear loose, comfortable clothing. You will be asked to sign a consent form before the test.
How the Test will Feel
Electrodes (conductive patches) will be placed on your chest, arms, and legs to record your heart's activity.
The blood pressure cuff on your arm will be inflated every few minutes, producing a squeezing sensation that may feel tight.
During the test, people feel chest discomfort, extra or skipped heartbeats, dizziness, headache, nausea, or shortness of breath. Be sure to tell the person doing the test if you feel any of these symptoms.
Why the Test is Performed
The test is performed to see whether your heart muscle is getting enough blood flow and oxygen when it is working hard (under stress).
Your provider may order this test if you:
- Have new symptoms of angina or chest pain
- Have angina that is getting worse
- Have recently had a heart attack
- Are going to have surgery or begin an exercise program, if you are at high risk for heart disease
- Have heart valve problems
The results of this stress test can help your provider:
- Determine how well a heart treatment is working and change your treatment, if needed
- Determine how well your heart is pumping
- Diagnose coronary artery disease
- See whether your heart is too large
Normal Results
A normal test will most often mean that you were able to exercise as long as or longer than most people of your age and sex. You also did not have symptoms or concerning changes in blood pressure and your ECG. Your heart pictures show that all parts of your heart respond to increased stress by pumping harder.
A normal result means that blood flow through the coronary arteries is probably normal.
The meaning of your test results depends on the reason for the test, your age, and your history of heart and other medical problems.
What Abnormal Results Mean
Abnormal results may be due to:
- Reduced blood flow to a part of your heart. The most likely cause is a narrowing or blockage of the arteries that supply your heart muscle.
- Scarring of your heart muscle due to a past heart attack.
After the test you may need:
-
Angioplasty and stent placement
Angioplasty and stent placement
The blood vessels that bring blood to your brain and face are called the carotid arteries. You have a carotid artery on each side of your neck. The...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Changes in your heart medicines
-
Coronary angiography
Coronary angiography
Coronary angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the arteries in your heart....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Heart bypass surgery
Heart bypass surgery
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to go around a blockage to reach your heart.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks
The risks are very low. Health care professionals will monitor you during the entire procedure.
Rare complications include:
-
Abnormal heart rhythm
Abnormal heart rhythm
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregul...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Fainting (syncope)
-
Heart attack
Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
References
Boden WE. Angina pectoris and stable ischemic heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 56.
Fowler GC, Smith A. Stress echocardiography. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 76.
Rader F, Siegel RJ. Stress echocardiography for detecting coronary ischemia. In: Otto CM, ed. Practice of Clinical Echocardiography. 6th ed. Philadelphia, PA: Elsevier; 2022;chap 19.
Van Der Bijl P, Bax JJ, Delgado V. Nonexercise stress echocardiography for the diagnosis of coronary disease. In: Otto CM, ed. Practice of Clinical Echocardiography. 6th ed. Philadelphia, PA: Elsevier; 2022:chap 20.
Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology joint committee on clinical practice guidelines. Circulation. 2023;148:e9–e119. PMID: 37471501 pubmed.ncbi.nlm.nih.gov/37471501/.
Wu JC, Gillam LD, Solomon SD, Bulwer B. Echocardiography. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 16.
-
Heart - section through the middle - illustration
The interior of the heart is composed of valves, chambers, and associated vessels.
Heart - section through the middle
illustration
-
Heart - front view - illustration
The external structures of the heart include the ventricles, atria, arteries and veins. Arteries carry blood away from the heart while veins carry blood into the heart. The vessels colored blue indicate the transport of blood with relatively low content of oxygen and high content of carbon dioxide. The vessels colored red indicate the transport of blood with relatively high content of oxygen and low content of carbon dioxide.
Heart - front view
illustration
-
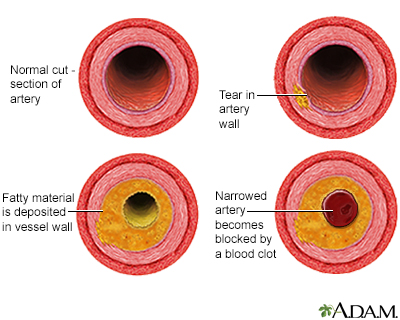
Developmental process of atherosclerosis - illustration
The development of arterial atherosclerosis may occur when deposits of cholesterol and plaque accumulate at a tear in the inner lining of an artery. As the deposits harden and occlude the arterial lumen, blood flow to distant tissues decreases and a clot may become lodged, completely blocking the artery.
Developmental process of atherosclerosis
illustration
-
Heart - section through the middle - illustration
The interior of the heart is composed of valves, chambers, and associated vessels.
Heart - section through the middle
illustration
-
Heart - front view - illustration
The external structures of the heart include the ventricles, atria, arteries and veins. Arteries carry blood away from the heart while veins carry blood into the heart. The vessels colored blue indicate the transport of blood with relatively low content of oxygen and high content of carbon dioxide. The vessels colored red indicate the transport of blood with relatively high content of oxygen and low content of carbon dioxide.
Heart - front view
illustration
-
Developmental process of atherosclerosis - illustration
The development of arterial atherosclerosis may occur when deposits of cholesterol and plaque accumulate at a tear in the inner lining of an artery. As the deposits harden and occlude the arterial lumen, blood flow to distant tissues decreases and a clot may become lodged, completely blocking the artery.
Developmental process of atherosclerosis
illustration
Review Date: 1/1/2023
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Internal review and update on 02/19/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.