Anterior vaginal wall repair
Anterior vaginal wall repair is a surgical procedure. This surgery tightens the front (anterior) wall of the vagina.
Anterior
Anterior means "in front of" or "the front surface of. " It usually refers to the front side of the body. For example, your knee caps are on the ant...

Description
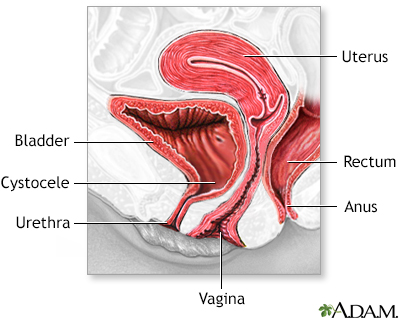
The anterior vaginal wall can sink (prolapse) or bulge. This occurs when the bladder or the urethra sink into the vagina.
The repair may be done while you are under:
- General anesthesia: You will be asleep and unable to feel pain.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark Article - Spinal anesthesia: You will be awake, but you will be numb from the waist down and you will not feel pain. You will be given medicines to help you relax.
Spinal anesthesia
Spinal and epidural anesthesia are procedures that deliver medicines that numb parts of your body to block pain. They are given through shots in or ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Your surgeon will:
- Make a surgical cut through the front wall of your vagina.
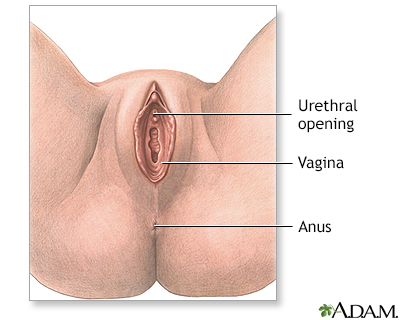
Vagina
The vagina is the female body part that connects the womb (uterus) and cervix to the outside of the body.
 ImageRead Article Now Book Mark Article
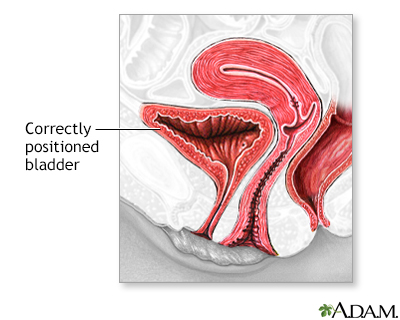
ImageRead Article Now Book Mark Article - Move your bladder back to its normal location.
- May fold your vagina, or cut away part of it.
- Put sutures (stitches) in the tissue between your vagina and bladder. These will hold the walls of your vagina in the correct position.
- Place a patch between your bladder and vagina. This patch can be made of commercially available biological material (cadaveric tissue). The FDA has banned use of synthetic material and animal tissue in the vagina to treat anterior vaginal wall prolapse.
- Attach sutures to the walls of the vagina to the tissue on the side of your pelvis.
Why the Procedure Is Performed
This procedure is used to repair sinking or bulging of the anterior vaginal wall.
Symptoms of anterior vaginal wall prolapse include:
Anterior vaginal wall prolapse
Uterine prolapse occurs when the womb (uterus) drops down and presses into the vaginal area.

- You may not be able to empty your bladder completely.
- Your bladder may feel full all the time.
- You may feel pressure in your vagina.
- You may be able to feel or see a bulging at the opening of the vagina.
- You may have pain when you have sex.
- You may leak urine when you cough, sneeze, or lift something.
- You may get bladder infections.
This surgery by itself does not treat stress incontinence. Stress incontinence is the leaking of urine when you cough, sneeze, or lift. Surgery to correct stress urinary incontinence may be performed along with other surgeries.
Stress incontinence
Stress urinary incontinence occurs when your bladder leaks urine during physical activity or exertion. It may happen when you cough, sneeze, lift so...

Before doing this surgery, your health care provider may have you:
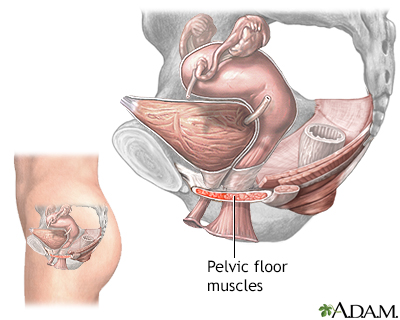
- Learn pelvic floor muscle exercises (Kegel exercises)
Kegel exercises
Kegel exercises can help make the pelvic floor muscles under the uterus, bladder, and bowel (large intestine) stronger. They can help both men and w...
Read Article Now Book Mark Article - Use estrogen cream in your vagina
- Try a device called a pessary in your vagina to strengthen the muscle around the vagina
Risks
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots
- Infection
Risks for this procedure include:
- Damage to the urethra, bladder, or vagina
- Irritable bladder
- Changes in the vagina (prolapsed vagina)
- Urine leakage from the vagina or to the skin (fistula)
- Worsening urinary incontinence
Urinary incontinence
Urinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Lasting pain
- Complications from the material used during surgery (mesh/grafts)
Before the Procedure
Always tell your surgeon what medicines you are taking. Also tell them about the medicines, supplements, or herbs you bought without a prescription that you are taking.
During the days before the surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), warfarin (Coumadin), and any other medicines that make it hard for your blood to clot.
- Ask your surgeon which medicines you should still take on the day of your surgery.
On the day of your surgery:
- You very often will be asked not to drink or eat anything for 6 to 12 hours before the surgery.
- Take the medicines your surgeon told you to take with a small sip of water.
- Your surgeon will tell you when to arrive at the hospital.
After the Procedure
You may have a catheter to drain urine for 1 or 2 days after surgery. You can start eating normal food soon after the surgery.
Catheter
A urinary catheter is a tube placed in the body to drain and collect urine from the bladder.

When your normal bowel function returns, you can return to your regular diet.
You should not insert anything in the vagina, lift heavy items, or have sex until your surgeon says it is OK.
Outlook (Prognosis)
This surgery will very often repair the prolapse and the symptoms will go away. This improvement will often last for years.
Reviewed By
Sovrin M. Shah, MD, Associate Professor, Department of Urology, The Icahn School of Medicine at Mount Sinai, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Kirby AC, Lentz GM. Pelvic organ prolapse, abdominal hernias, and inguinal hernias: diagnosis and management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 20.
Winters JC, Krlin RM, Hallner B. Vaginal and abdominal reconstructive surgery for pelvic organ prolapse. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 124.
Wolff GF, Winters JC, Krlin RM. Anterior pelvic organ prolapse repair. In: Smith JA Jr, Howards SS, Preminger GM, Dmochowski RR, eds. Hinman's Atlas of Urologic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 89.


 All rights reserved.
All rights reserved.