Skin care and incontinence
Incontinence - skin care; Incontinence - pressure sore; Incontinence - pressure ulcer; Incontinence - bed soreA person with incontinence is not able to prevent urine and stool from leaking. This can lead to skin problems near the buttocks, hips, genitals, and between the pelvis and rectum (perineum).
Information
People who have problems controlling their urine or bowels (called incontinence) are at risk for skin problems. The skin areas most affected are near the buttocks, hips, genitals, and between the pelvis and rectum (perineum).
Urine
Urinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries ...

Bowels
Bowel incontinence is the loss of bowel control, causing you to unexpectedly pass stool. This can range from sometimes leaking a small amount of sto...

Excess moisture in these areas makes skin problems such as redness, peeling, irritation, and yeast infections likely.
Yeast infections
Candida infection of the skin is a yeast infection of the skin. The medical name of the condition is cutaneous candidiasis.

Bedsores (pressure sores) may also develop if a person:
Pressure sores
A pressure sore is an area of the skin that breaks down when something keeps rubbing or pressing against the skin.

- Has not been eating well (is malnourished)
Malnourished
Malnutrition is the condition that occurs when your body does not get enough nutrients.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Received radiation therapy to the area
Radiation therapy
Radiation therapy uses high-powered radiation (such as x-rays or gamma rays), particles, or radioactive seeds to kill cancer cells.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spends most or all of the day in a wheelchair, regular chair, or bed without changing position
TAKING CARE OF THE SKIN
Using diapers and other products can make skin problems worse. Although they may keep bedding and clothing cleaner, these products allow urine or stool to be in constant contact with the skin. Over time, the skin breaks down. Special care must be taken to keep the skin clean and dry. This can be done by:
- Cleaning and drying the area right away after urinating or having a bowel movement.
- Cleaning the skin with mild, dilute soap and water then rinsing well and gently patting dry.
Use soap-free skin cleansers that do not cause dryness or irritation. Follow the product's instructions. Some products do not require rinsing.
Moisturizing creams can help keep the skin moist. Avoid products that contain alcohol, which may irritate the skin. If you are receiving radiation therapy, ask your health care provider if it is OK to use any creams or lotions.
Consider using a skin sealant or moisture barrier. Creams or ointments that contain zinc oxide, lanolin, or petrolatum form a protective barrier on the skin. Some skin care products, often in the form of a spray or a towelette, create a clear, protective film over the skin. Your provider can recommend barrier creams to help protect the skin.
Even if these products are used, the skin must still be cleaned each time after passing urine or stool. Reapply the cream or ointment after cleaning and drying the skin.
Incontinence can cause a yeast infection on the skin. This is an itchy, red, pimple-like rash. The skin may feel raw. Products are available to treat a yeast infection:
- If the skin is moist most of the time, use a powder with antifungal medicine, such as nystatin or miconazole. Do not use baby powder.
- A moisture barrier or skin sealant may be applied over the powder.
- If severe skin irritation develops, contact your provider.
- If bacterial infection occurs, antibiotics applied to the skin or taken by mouth may help.
The National Association for Continence (NAFC) has helpful information at www.nafc.org.
IF YOU ARE BEDRIDDEN OR USING A WHEELCHAIR
Check your skin for pressure sores every day. Look for reddened areas that do not turn white when pressed. Also look for blisters, sores, or open ulcers. Tell your provider if there is any foul-smelling drainage.
A healthy, well-balanced diet that contains enough calories and protein helps keep you and your skin healthy.
For people who must stay in bed:
- Change your position often, at least every 2 hours
- Change sheets and clothing right away after they are soiled
- Use items that can help reduce pressure, such as pillows or foam padding
For people in a wheelchair:
- Make sure your chair fits properly
- Shift your weight every 15 to 20 minutes
- Use items that can help reduce pressure, such as pillows or foam padding
Smoking affects healing of the skin, so stopping smoking is important.
References
Bliss DZ, Mathiason MA, Gurvich O, et al. Incidence and predictors of incontinence associated skin damage in nursing home residents with new onset incontinence. J Wound Ostomy Continence Nurs. 2017;44(2):165-171. PMID: 28267124 pubmed.ncbi.nlm.nih.gov/28267124/.
Boyko TV, Longaker MT, Yang GP. Review of the current management of pressure ulcers. Advances in Wound Care (New Rochelle). 2018;7(2):57-67. PMID: 29392094 pubmed.ncbi.nlm.nih.gov/29392094/.
Harper A, Wilkinson I, Preston Jo. Geriatric medicine, frailty and multimorbidity. In: Feather A, Randall D, Waterhouse M, eds. Kumar and Clark's Clinical Medicine. 10th ed. Philadelphia, PA: Elsevier; 2021:chap 15.
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Dermatoses resulting from physical factors. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 3.
Khansa I, Janis JE. Pressure sores. In: Song DH, Hong JP, eds. Plastic Surgery: Volume 4: Lower Extremity, Trunk, and Burns. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 16.
-
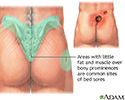
Areas where bedsores occur - illustration
Bedsores, also known as pressure sores or decubitis ulcers, are a breakdown and ulceration of tissue due to a combination of the weight of the body on the surface of the skin and the friction of a resistant surface such as a bed. Areas where bony prominences are less padded by muscle and fat, such as the hip bones, tailbone and heels of the feet, are most susceptible to bedsores. Non-mobile patients are vulnerable to the formation pressure sores when left lying for long periods of time in the same prone position.
Areas where bedsores occur
illustration
-
Areas where bedsores occur - illustration
Bedsores, also known as pressure sores or decubitis ulcers, are a breakdown and ulceration of tissue due to a combination of the weight of the body on the surface of the skin and the friction of a resistant surface such as a bed. Areas where bony prominences are less padded by muscle and fat, such as the hip bones, tailbone and heels of the feet, are most susceptible to bedsores. Non-mobile patients are vulnerable to the formation pressure sores when left lying for long periods of time in the same prone position.
Areas where bedsores occur
illustration
-
Urinary incontinence - InDepth
(In-Depth)
Review Date: 2/15/2024
Reviewed By: Elika Hoss, MD, Assistant Professor of Dermatology, Mayo Clinic, Scottsdale, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.