Walking abnormalities
Gait abnormalitiesWalking abnormalities can be caused by many different types of problems. Problems with the joints, (such as arthritis), bones (such as deformities), circulation (such as peripheral vascular disease), or even pain can make it difficult to walk properly. Diseases or injuries to the nerves, muscles, brain, spinal cord, or inner ear can affect normal walking.
Arthritis
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of...

Considerations
The pattern of how a person walks is called the gait. Different types of walking problems occur without a person's control. Most, but not all, are due to a physical condition.
Some walking abnormalities have been given names:
- Propulsive gait -- a stooped, stiff posture with the head and neck bent forward.
- Spastic gait -- a stiff, foot-dragging walk caused by a long muscle contraction on one side.
- Scissoring gait -- legs flexed slightly at the hips and knees like crouching, with the knees and thighs hitting or crossing in a scissors-like movement. A scissoring gait is often a more severe form of a spastic gait.
- Steppage gait -- foot drop where the foot hangs with the toes pointing down, causing the toes to scrape the ground while walking, requiring someone to lift the leg higher than normal when walking.
- Waddling gait -- a duck-like walk that may appear in childhood or later in life.
- Ataxic, or broad-based, gait -- feet wide apart with irregular, jerky, and weaving or slapping when trying to walk.
- Magnetic gait -- shuffling with feet feeling as if they stick to the ground.
- Antalgic gait -- when pain prevents the normal motion of the feet or legs.
- Shuffling gait -- when the feet don't lift normally and slide on the ground, often due to Parkinson disease.
Causes
Abnormal gait may be caused by diseases in different areas of the body.
General causes of abnormal gait may include:
- Arthritis of the spine, hip, leg, or foot joints
-
Conversion disorder (a mental disorder)
Conversion disorder
Functional neurological disorder (FND) is a condition in which there is a problem with how the brain receives and sends information to one or more pa...
Read Article Now Book Mark Article - Foot problems (such as a callus, corn, ingrown toenail, wart, pain, skin sore, swelling, or spasms)
- Broken bone
- Injections into muscles that cause soreness in the leg or buttocks
- Infection
- Injury
- Legs that are of different lengths
- Inflammation or swelling of the muscles (myositis)
Myositis
Myositis is an inflammation or swelling of the muscles. It is most often caused by injury, infection, medicines, or an autoimmune disorder. Dermatom...
Read Article Now Book Mark Article -
Shin splints
Shin splints
Shin splints can cause pain in the front of your lower leg. The pain of shin splints is from the inflammation of the muscles, tendons, and bone tiss...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Shoe problems
- Inflammation or swelling of the tendons (tendinitis)
Tendinitis
Tendons are the fibrous structures that join muscles to bones. When these tendons become swollen or inflamed, it is called tendinitis. In many case...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Brain, spinal cord, and peripheral nerve diseases
- Vision problems
- Inner ear problems
This list does not include all causes of abnormal gait.
CAUSES OF SPECIFIC GAITS
Propulsive gait:
-
Carbon monoxide poisoning
Carbon monoxide poisoning
Carbon monoxide is an odorless gas that causes thousands of deaths each year in North America. Breathing in carbon monoxide is very dangerous. It i...
Read Article Now Book Mark Article - Manganese poisoning
-
Parkinson disease
Parkinson disease
Parkinson disease results from certain brain cells dying. These cells help control movement and coordination. The disease leads to shaking (tremors...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Use of certain medicines, including phenothiazines, haloperidol, loxapine, and metoclopramide (usually, medicine effects are temporary)
Spastic or scissoring gait:
- Autoimmune disorders such as systemic lupus
-
Brain abscess
Brain abscess
A brain abscess is a collection of pus, immune cells, and other material in the brain, caused by a bacterial or fungal infection.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Brain or head trauma
Brain or head trauma
A head injury is any trauma to the scalp, skull, or brain. Head injury can be either closed or open (penetrating). A closed head injury means you rec...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Brain tumor
Brain tumor
A brain tumor is a group (mass) of abnormal cells that grow in the brain. This article focuses on primary brain tumors in children.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Stroke
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Cerebral palsy
Cerebral palsy
Cerebral palsy (CP) is a group of disorders that involve the brain. This affects nervous system functions, such as movement, learning, hearing, seei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Cervical spondylosis with myelopathy (a problem with the vertebrae in the neck)
Cervical spondylosis
Cervical spondylosis is a disorder in which there is wear on the cartilage (disks) and bones of the neck (cervical vertebrae). It is a common cause ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infections such as Lyme disease, syphilis, HIV, and others
- Liver failure
-
Multiple sclerosis (MS)
Multiple sclerosis
Multiple sclerosis (MS) is an autoimmune disease that affects the brain and spinal cord (central nervous system).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal cord trauma
Spinal cord trauma
Spinal cord trauma is damage to the spinal cord. It may result from direct injury to the cord itself or indirectly from disease of the nearby bones,...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Spinal cord tumor
Tumor
A tumor is an abnormal growth of body tissue. Tumors can be cancerous (malignant) or noncancerous (benign).
Read Article Now Book Mark Article -
Neurosyphilis (bacterial infection of the brain or spinal cord due to syphilis)
Neurosyphilis
Neurosyphilis is a bacterial infection of the brain or spinal cord. It usually occurs in people who have had untreated syphilis for many years....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Syringomyelia (collection of cerebrospinal fluid that forms in the spinal cord)
Syringomyelia
Syringomyelia is a cyst-like collection of cerebrospinal fluid (CSF) that forms in the spinal cord. Over time, it may damage the spinal cord....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vitamin or mineral deficiency (low vitamin B12, vitamin E, or copper levels)
Steppage gait:
- Neuropathy such as Guillain-Barre syndrome and hereditary neuropathy
Guillain-Barre syndrome
Guillain-Barré syndrome (GBS) is a serious health problem that occurs when the body's defense (immune) system mistakenly attacks part of the peripher...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
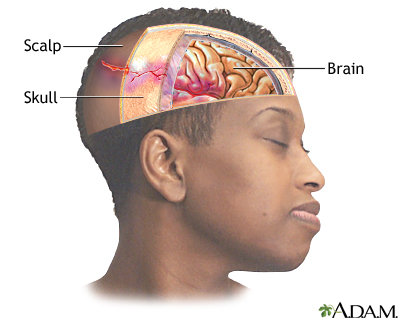
Herniated lumbar disk
Herniated lumbar disk
A herniated (slipped) disk occurs when all or part of a disk is forced through a weakened part of the disk. This may place pressure on nearby nerves...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Multiple sclerosis
- Muscle weakness of the lower leg
-
Peroneal neuropathy
Peroneal neuropathy
Common peroneal nerve dysfunction is due to damage to the peroneal nerve leading to loss of movement or sensation in the foot and leg. This conditio...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Polio
Polio
Polio is a viral disease that can affect nerves and can lead to partial or full paralysis. The medical name for polio is poliomyelitis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal cord injury
Spinal cord injury
The spinal cord contains the nerves that carry messages between your brain and the rest of the body. The cord passes through your neck and back. A ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Muscle diseases
The conditions that cause spastic or scissoring gait can also cause steppage gait.
Waddling gait:
-
Congenital hip dysplasia
Congenital hip dysplasia
Developmental dysplasia of the hip (DDH) is a dislocation of the hip joint that is present at birth. The condition is found in babies or young child...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Muscular dystrophy (a group of inherited disorders that cause muscle weakness and loss of muscle tissue)
Muscular dystrophy
Muscular dystrophy (MD) is a group of inherited disorders that cause muscle weakness and loss of muscle tissue, which get worse over time.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Muscle disease (myopathy)
-
Spinal muscle atrophy
Spinal muscle atrophy
Spinal muscular atrophy (SMA) is a group of disorders of the motor neurons (motor cells). These disorders are passed down through families (inherite...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Ataxic, or broad-based, gait:
-
Cerebellar ataxia (uncoordinated muscle movement due to disease or injury to the cerebellum in the brain)
Cerebellar ataxia
Acute cerebellar ataxia is the sudden inability to coordinate muscle movement due to disease or injury to the cerebellum. This is the area in the br...
Read Article Now Book Mark Article - Chiari or other malformation
- Alcohol intoxication
- Brain injury
- Progressive damage to nerve cells in the cerebellum of the brain (cerebellar degeneration)
- Medicines (phenytoin and other anti-seizure medicines)
- Polyneuropathy (damage to many nerves, as occurs with diabetes)
- Stroke or bleeding in the cerebellum
Magnetic gait:
- Disorders that affect the front part of the brain
-
Hydrocephalus (increased fluid in the brain)
Hydrocephalus
Hydrocephalus is a buildup of fluid inside the skull that leads to the brain pushing against the skull. Hydrocephalus means "water on the brain. "...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Home Care
Treating the underlying cause often improves the gait. For example, gait abnormalities from trauma to part of the leg will improve as the leg heals.
Physical therapy almost always helps with short-term or long-term gait disorders. Therapy will reduce the risk for falls and other injuries. A physical therapist can also determine if assistive devices would help your gait.
For an abnormal gait that occurs with conversion disorder, counseling and support from family members are strongly recommended.
For any gait problem that is likely to be long term, reduce fall risk by modifying one's surroundings. Keep pathways well-lit and free of clutter like wires and other hazards. Remove loose rugs and install grab bars or railings.
Reduce fall risk
Older adults and people with medical problems are at risk of falling or tripping. This can result in broken bones or more serious injuries. Use the ...

For a propulsive gait:
- Encourage the person to be as independent as possible.
- Allow plenty of time for daily activities, especially walking. People with this problem are likely to fall because they have poor balance and are always trying to catch up.
- Provide walking assistance for safety reasons, especially on uneven ground.
- See a physical therapist for exercise therapy and walking retraining.
For a scissoring or spastic gait:
- People with a scissoring gait often lose skin sensation. Skin care should be used to avoid skin sores.
- Leg braces and in-shoe splints can help keep the foot in the right position for standing and walking. A physical therapist can supply these and provide exercise therapy, if needed.
- Exercises are encouraged.
- A cane or a walker is recommended for those with poor balance.
- Medicines (muscle relaxers, anti-spasticity medicines) can reduce the muscle overactivity.
For a steppage gait:
- Get enough rest. Fatigue can often cause a person to stub a toe and fall.
- Leg braces or orthoses and in-shoe splints can help keep the foot in the best position for standing and walking. A physical therapist can supply these and provide exercise therapy, if needed. For some, a high-top boot may be sufficient.
For a waddling gait, follow the treatment your health care provider prescribed. Bracing, canes and walkers can be of help.
For a magnetic gait due to hydrocephalus, walking may improve after the excess fluid is treated.
When to Contact a Medical Professional
If there is any sign of uncontrollable and unexplained gait abnormalities, contact your provider.
What to Expect at Your Office Visit
Your provider will take a medical history and perform a physical exam.
Medical history questions may include:
- Time pattern, such as when the problem started, and if it came on suddenly or gradually
- Type of gait disturbance, such as any of those mentioned above
- Other symptoms, such as pain and its location, paralysis, and whether there's been a recent infection
- What medicines you take
- Injury history, such as leg, head, or spinal injury
- Other illnesses such as polio, tumors, stroke, or other blood vessel problems
- If there have been recent treatments such as vaccinations, surgery, chemotherapy, or radiation therapy
- Self and family history, such as birth defects, diseases of the nervous system, growth problems, problems of the spine
The physical exam will include muscle, bone, and nervous system examination. Your provider will decide which tests to do based on the results of the physical exam.
In complex cases, a computer-assisted gait analysis may be done.
References
Magee DJ, Manske RC. Assessment of gait. In: Magee DJ, Manske RC, eds. Orthopedic Physical Assessment. 7th ed. St Louis, MO: Elsevier; 2021:chap 14.
Thompson PD, Nutt JG. Gait disorders. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 25.
-
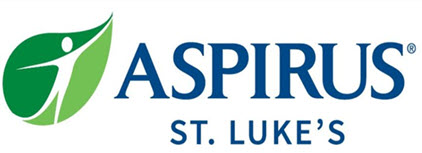
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
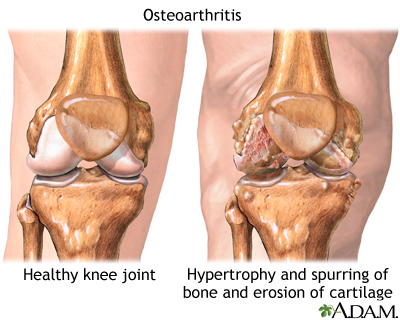
Head injury - illustration
Head injuries can range from a minor bump on the head to a devastating brain injury. Learning to recognize a serious head injury, and implementing basic first aid, can make the difference in saving someones life. Common causes of head injury include traffic accidents, falls, physical assault, and accidents at home, work, outdoors, or while playing sports.
Head injury
illustration
-
Herniated lumbar disk - illustration
Herniated lumbar disk is a condition in which part or all of the soft, gelatinous central portion of an intervertebral disk (the nucleus pulposus) is forced through a weakened part of the disk, resulting in back pain and nerve root irritation.
Herniated lumbar disk
illustration
-
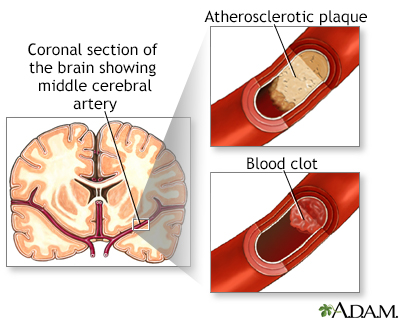
Stroke - illustration
A stroke involves loss of brain functions caused by a loss of blood circulation to areas of the brain. The blockage usually occurs when a clot or piece of atherosclerotic plaque breaks away from another area of the body and lodges within the vasculature of the brain.
Stroke
illustration
-
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
Head injury - illustration
Head injuries can range from a minor bump on the head to a devastating brain injury. Learning to recognize a serious head injury, and implementing basic first aid, can make the difference in saving someones life. Common causes of head injury include traffic accidents, falls, physical assault, and accidents at home, work, outdoors, or while playing sports.
Head injury
illustration
-
Herniated lumbar disk - illustration
Herniated lumbar disk is a condition in which part or all of the soft, gelatinous central portion of an intervertebral disk (the nucleus pulposus) is forced through a weakened part of the disk, resulting in back pain and nerve root irritation.
Herniated lumbar disk
illustration
-
Stroke - illustration
A stroke involves loss of brain functions caused by a loss of blood circulation to areas of the brain. The blockage usually occurs when a clot or piece of atherosclerotic plaque breaks away from another area of the body and lodges within the vasculature of the brain.
Stroke
illustration
Review Date: 2/11/2025
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.