Urination - difficulty with flow
Delayed urination; Hesitancy; Difficulty initiating urinationDifficulty starting or maintaining a urine stream is called urinary hesitancy.
Considerations
Urinary hesitancy affects people of all ages and occurs in both sexes. However, it is most common in older men with an enlarged prostate gland.
Enlarged prostate
The prostate is a gland that produces some of the fluid that carries sperm during ejaculation. The prostate gland surrounds the urethra, the tube th...

Urinary hesitancy most often develops slowly over time. You may not notice it until you are unable to urinate (called urinary retention). This causes swelling and discomfort in your bladder.
Causes
The most common cause of urinary hesitancy in older men is an enlarged prostate. Almost all older men have some trouble with dribbling, weak urine stream, and starting urination.
Another common cause is infection of the prostate or urinary tract. Symptoms of a possible infection include:
- Burning or pain with urination
- Frequent urination
- Cloudy urine
- Sense of urgency (strong, sudden urge to urinate)
- Blood in the urine
The problem can also be caused by:
- Some medicines (such as remedies for colds and allergies, tricyclic antidepressants, some medicines used for incontinence, and some vitamins and supplements)
- Nervous system disorders or problems with the spinal cord
- Side effects of surgery
- Scar tissue (stricture) in the tube leading from the bladder (urethra)
- Spastic muscles in the pelvis
Home Care
Steps you can take to care for yourself include:
- Keep track of your urination patterns and bring the report to your health care provider.
- Apply heat to your lower abdomen (below your belly button and above the pubic bone). This is where the bladder sits. The heat relaxes muscles and aids urination.
- Massage or apply light pressure over your bladder to help the bladder empty.
- Take a warm bath or shower to help stimulate urination.
When to Contact a Medical Professional
Call your provider if you notice urinary hesitancy, dribbling, or a weak urine stream.
Call your provider right away if:
- You have a fever, vomiting, side or back pain, shaking chills, or are passing little urine for 1 to 2 days.
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleVomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You have blood in your urine, cloudy urine, a frequent or urgent need to urinate, or a discharge from the penis or vagina.
- You are unable to pass urine.
What to Expect at Your Office Visit
Your provider will take your medical history and do an exam to look at your pelvis, genitals, rectum, abdomen, and lower back.
You may be asked questions such as:
- How long have you had the problem and when did it start?
- Is it worse in the morning or at night?
- Has the force of your urine flow decreased? Do you have dribbling or leaking urine?
- Does anything help or make the problem worse?
- Do you have symptoms of an infection?
- Have you had other medical conditions or surgeries that could affect your urine flow?
- What medicines do you take?
Tests that may be performed include:
- Blood urea nitrogen test
- Creatinine (serum)
- Electrolytes (serum)
- Catheterization of the bladder to determine how much urine remains in your bladder after trying to urinate and to get urine for culture (a catheterized urine specimen)
-
Cystometrogram or urodynamic study
Cystometrogram
A cystometric study measures the amount of fluid in the bladder when you first feel the need to urinate, when you are able to sense fullness, and whe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Transrectal ultrasound of the prostate
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urethral swab for culture
-
Urinalysis and culture
Urinalysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Voiding cystourethrogram
Voiding cystourethrogram
A voiding cystourethrogram is an x-ray study of the bladder and urethra. It is done while the bladder is emptying.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - A bladder scan and ultrasound (measures urine left behind without catheterization)
-
Cystoscopy
Cystoscopy
Cystoscopy is a surgical procedure. This is done to see the inside of the bladder and urethra using a thin, lighted tube.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment for urinary hesitancy depends on the cause, and may include:
- Medicines to relieve the symptoms of an enlarged prostate.
- Antibiotics to treat any infection. Be sure to take all your medicines as directed.
- Surgery to relieve a prostate blockage (transurethral resection of the prostate, TURP).
TURP
Transurethral resection of the prostate (TURP) is a surgery to remove the inside part of the prostate gland. It is done in order to treat symptoms o...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Procedure to dilate or cut scar tissue in the urethra.
References
Elsamra SE. Evaluation of the urologic patient: history and physical examination. In: Partin AW, Domochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 1.
Smith PP, Kuchel GA. Aging of the urinary tract. In: Fillit HM, Rockwood K, Young J, eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8th ed. Philadelphia, PA: Elsevier, 2017:chap 22.
-
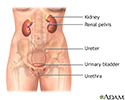
Female urinary tract - illustration
The female and male urinary tracts are relatively the same except for the length of the urethra.
Female urinary tract
illustration
-
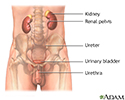
Male urinary tract - illustration
The male and female urinary tracts are relatively the same except for the length of the urethra.
Male urinary tract
illustration
-
Female urinary tract - illustration
The female and male urinary tracts are relatively the same except for the length of the urethra.
Female urinary tract
illustration
-
Male urinary tract - illustration
The male and female urinary tracts are relatively the same except for the length of the urethra.
Male urinary tract
illustration
Review Date: 7/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.